Serious Bacteria Infections
Source: ME Primer for Healthcare Professionals: based on Myalgic encephalomyelitis: International Consensus Criteria, 2012
Undiagnosed Lyme disease often called ME or CFS
- Gustaw K. Chronic fatigue syndrome following tick-borne diseases.Neurol Neurochir Pol.2003;37:1211–21. 71% of ME/CFS cases had Lyme infection.
- Chronic Fatigue Syndrome Patients Subsequently Diagnosed with Lyme Disease Borrelia burgdorferi: Evidence for Mycoplasma species Co-Infections Garth L. Nicolson, PhD, Nancy L. Nicolson, PhD and Joerg Haier, MD, PD, Journal of Chronic Fatigue Syndrome 2008; 14(4):5-17
- Several Bacteria and ME / CFS scientific research papers at http://www.immed.org/fatigue_illness_research.html
- RETROSPECTIVE ANALYSIS OF A COHORT OF INTERNATIONALLY CASE DEFINED CHRONIC FATIGUE SYNDROME PATIENTS IN A LYME ENDEMIC AREA.. Samuel Shor, MD, FACP
- Treib, J., Grauer, M.T., Haas, A., Langenbach, J., Holzer, G.,Woessner, R. Chronic Fatigue Syndrome in patients with Lyme borreliosis Eur Neurol. 2000; 43(2): 107 - 9
- Nicolson GL, and Nicolson NL. Chronic infections as a common etiology for many patients with chronic fatigue syndrome, fibromyalgia, and Gulf War Illness. Intern J Med. 1998; 1:42-6.
- Taylor, S. Lyme disease (borreliosis). A plague of ignorance regarding the ignorance of a plague. http://www.autoimmunityresearch.org/lyme-disease/
- In a presentation to the Edinburgh ME group in September 2005, Professor John Gow of Glasgow University stated that gene expression regulation in those with ME is identical to that seen in Lyme patients.
- Relationship between Lyme Disease and CFS. Critical Needs and Gaps in Understanding Prevention, Amelioration, and Resolution of Lyme and Other Tick-Borne Diseases: The Short-Term and Long-Term Outcomes - Workshop Report. Released: April 20, 2011
- Donta, S. Lyme disease as a model of Chronic Fatigue Syndrome. CFS Res Rev. 2002; 3(2): 1 - 4
- Goldenberg, D.L. Fibromyalgia, chronic fatigue syndrome, and myofascial pain syndrome. Curr Opin Rheumatol. 1995; 7(2): 127 - 35
- Reponse to Dr. Ho-Yen in Scotland regarding Lyme and ME / CFS
- Evidence from Dr Hugh Derham, Australia
'
Dr Hugh Derham has seen it all before. The Perth practitioner is one of only a handful of so-called “Lyme-literate” GPs risking their professional reputation by diagnosing patients with the disease. He says he has more than 400 people on his books who have tested positive for Lyme, ranging from three years old to 82. About 10 per cent of them have never left Australia.
With an interest in chronic fatigue syndrome (CFS), myalgic encephalomyelitis (ME) and fibromyalgia, over the past three years, he has tested 300 of his most chronic cases in accredited labs both here and overseas. Some 95 per cent of them have shown positive for varying types of Borrelia — proof, he says, that the illness lives up to its name, “The Great Imitator”, mimicking and manifesting diseases such as Parkinson’s, Alzheimer’s and multiple sclerosis (MS) that have no known cure.
“The first test most doctors do is just for the antibodies against Lyme disease and they are usually negative. But when you go looking further with superior PCR (polymerase chain reaction) or lymphocyte transformation testing or an immunoblot, usually you turn up a positive,” Derham says. “Thousands of Australians have Lyme disease and don’t know it.”
Read news article at
Lyme disease — a ticking timebomb that health authorities say does not exist
- Evidence from Dr Samuel Shor, USA
- See paper at RETROSPECTIVE ANALYSIS OF A COHORT OF INTERNATIONALLY CASE DEFINED CHRONIC FATIGUE SYNDROME PATIENTS IN A LYME ENDEMIC AREA
Results: Of the total 210 included in the analysis, 209 or 99% were felt to represent a high likelihood of “seronegative Lyme disease.” Initiating various antimicrobial regimen, involved at least a 50% improvement in clinical status in 130 or 62%. Although not achieving the 50% threshold according to the criteria discussed, another 55 patients subjectively identified a beneficial clinical response to antimicrobials, representing a total of 188 or 88% of the total identified as having a high potential for seronegative Lyme disease.
Conclusions: A potentially substantial proportion of patients with what would otherwise be consistent with internationally case defined CFS in a Lyme endemic environment actually have a perpetuation of their symptoms driven by a persistent infection by Borrelia burgdorferi. By treating this cohort with appropriately directed antimicrobials, we have the ability to improve outcomes.
- This is verified in another paper Lyme Disease Presenting as Chronic Fatigue Syndrome
- Evidence from Dr Kenny de Meirleir, Belgium
-
Evidence presented by Dr. Richard Horowitz to the Belgian Parliament
The following presentation was made to the Belgian Parliament in June 2014 by Dr. Richard Horowitz, an American medical doctor who has treated over 12,000 patients with Chronic Lyme, CFS, and other infectious diseases
https://www.youtube.com/watch?v=JSx3KdFaupA&t=8m40s
- Inadequate Lab tests for Chronic Lyme disease
Two comprehensive reviews of the accuracy of standard tests for Lyme, in Europe (1) and the US (2), showed that the same sample of blood could test positive or negative depending on which lab it was sent to, or even if tested again in the same lab. Worse still for those with suspected Borrelia infections, the Polish National Institute of Health has reported that patients with low or negative antibody levels have tested positive using other more sensitive techniques. Specific DNA capture and culturing showed that there were live bacteria in their body fluids (3) indicating that those with negative blood tests could be even more ill than those who have circulating antibodies. The problem of co-infections with other organisms is another complicating factor.
- Hunfeld, K.P., Stanek, G., Straube, E., Hagedorne, H-J., et al. Quality of Lyme serology. Wien Klin Wochenschr. 2002; 114(13-14): 591 - 600
- Bakken, L.L., Callister, S.M., Wand, P.J., Schell, R.F. Interlaboratory comparison of test results for detection of Lyme disease by 516 participants in the Wisconsin State Laboratory of Hygiene/ College of American Pathologists proficiency-testing program. J Clin Microbiol. 1997; 35:537 – 43
- Tylewska-Wierzbanowska, S., Chmielewski, T. Limitation of serological testing for Lyme borreliosis: Evaluation of ELISA and Western blot in comparison with PCR and culture methods. Wien Klin Wochenschr. 2002; 114(13-14): 601 - 5
- Factors affecting duration of chronic fatigue syndrome in pediatric patients. Petrov D, Marchalik D, Sosin M, Bal A.. Indian J Pediatr. 2012 Jan;79(1):52-5.
- Does Chronic Lyme disease exist ?
- Findings of Dr. Daniel Cameron and other doctors
- Research papers
- Research Listings
- Important new research papers
Cameron DJ, Johnson LB, Maloney EL. Evidence assessments and guideline recommendations in Lyme disease: the clinical management of known tick bites, erythema migrans rashes and persistent disease. Expert Rev Anti Infect Ther, 1-33 (2014)
Tseng YJ, Cami A, Goldmann DA, DeMaria A, Jr., Mandl KD. Incidence and Patterns of Extended-Course Antibiotic Therapy in Patients Evaluated for Lyme Disease. Clin Infect Dis, (2015).
- Evidence assessments and guideline recommendations in Lyme disease: the clinical management of known tick bites, erythema migrans rashes and persistent disease. DOI:10.1586/14787210.2014.940900. Daniel J Cameron, Lorraine B Johnson & Elizabeth L Maloney
pages 1103-1135
- Nicolson et al found a high prevalence of mycoplasmal (52%), Chlamydia pneumoniae (7.5%), and active HHV-6 (30.5%) infections in 200 CFS patients.
- Dr. Marshall's research and clinical findings
VDR abnormalities accompanied by pathogen infections, including Microbiota of bacteria which include L-form, biofilm, and intracellular bacterial forms. See http://mpkb.org/home/diseases/cfs
- "Organisms of two strains of the
Bethesda-Ballerup paracolon group were
isolated from feces from twelve of thirty-eight
nurses examined and from only one of fifty-
four persons who were
on the hospital staff at
the time of the epidemic and remained well. H
and O serum agglutinins against the Bethesda-Ballerup group (at a titre of 1:40 or more) were
found in twenty-two of forty-seven affected
nurses and in three of twenty-seven control
subjects. In eleven affected nurses a rise and
fall in titre was demonstrated during the period
of observation."
The Clinical Syndrome Variously Called Benign Myalgic Encephalomyelitis, Iceland Disease and Epidemic Neuromyasthenia. Dr. Acheson, American Journal of Medicine, 1959.
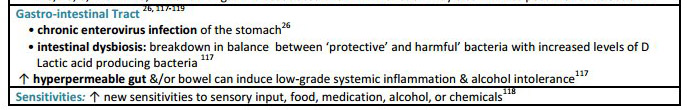
- Sheedy JR,
Wettenhall RE, Scanion D, Gooley PR, Lewis DP, McGregor N, Stapleton DI, Butt HL, De Meirleir KL.
Increased D-lactic acid intestinal
bacteria in patients with chronic fatigue syndrome.
In Vivo
2009;
23:
621-8.
- Lerner M, Beqaj S, Fitzgerald JT, Gill K, Gill C, Edington J (2010), "Subset-directed antiviral treatment of 142 herpesvirus patients with chronic fatigue syndrome", Virus Adaptation and Treatment, mei, Volume 2010:2, p.47-57
- Levine S (2001), "Prevalence in the cerebro spinal fluid of the following infectious agents in a cohort of 12 CFS subjects: Human Herpes Virus 6 & 8; Chlamydia Species; Mycoplasma Species, EBV; CMV and Coxsackie B Virus", Journal of Chronic Fatigue Syndrome, 9:91-2:41-51
- Maes M, Coucke F, Leunis JC: Normalization of the increased translocation of endotoxin from Gram negative enterobacteria (leaky gut) is accompanied by a remission of chronic fatigue syndrome. Neuro Endocrinol Lett 2007, 28:739-744.
- Nicolson et al showed that multiple co-infections (Mycoplasma, Chlamydia, HHV-6) in blood of chronic fatigue syndrome patients are associated with signs and symptoms: “Differences in bacterial and/or viral infections in (ME)CFS patients compared to controls were significant…The results indicate that a large subset of (ME)CFS patients show evidence of bacterial and/or viral infection(s), and these infections may contribute to the severity of signs and symptoms found in these patients” (Nicolson GL et al. APMIS 2003:111(5):557-566).
- High histamine levels in the intestines can be caused by bad bacteria or intestinal dysbiosis. Histamine can increase inflammation in the gut and elsewhere in the body, reduce digestion and absorption and adversely affect the immune system and worsen the symptoms of ME. High histamine levels are commonly found in ME patients. It is a good indicator of intestinal dysbiosis.
- Identification of a proton-chloride antiporter (EriC) by Himar1 transposon mutagenesis in Lactobacillus reuteri and its role in histamine production.
Hemarajata P, Spinler JK, Balderas MA, Versalovic J.
- Lactobacillus reuteri-specific immunoregulatory gene rsiR modulates histamine production and immunomodulation by Lactobacillus reuteri. Hemarajata P, Gao C, Pflughoeft KJ, Thomas CM, Saulnier DM, Spinler JK, Versalovic J.
- Effect of chemico-physical parameters on the histidine decarboxylase (HdcA) enzymatic activity in Streptococcus thermophilus PRI60.
Tabanelli G, Torriani S, Rossi F, Rizzotti L, Gardini F.
- Isolation and characterization of histamine-producing bacteria from fermented fish products. Moon JS, Kim SY, Cho KJ, Yang SJ, Yoon GM, Eom HJ, Han NS.
- Tyrosine- and histidine-decarboxylase positive lactic acid bacteria and enterococci in dry fermented sausages. Komprda T, Sládková P, Petirová E, Dohnal V, Burdychová R.
- PubMed articles on histamine and gut bacteria
- Staphylococci infections of the nose - "the majority of such
strains (Staphylococci) that are isolated by QML and S & N have
turned out to be toxin-producing strains .............. Once this
toxin is swallowed it may well have neurotoxic effects on the bowel's
nervous system. Also, if it is absorbed into the body, it may also
have toxic effects elsewhere. Thus, irritable bowel syndrome and even
CFS itself may well be related to infection of the nose by these
particular staphylococci as much of the research at Newcastle
University strongly suggests."
Dr. John Whiting, Dr Philip
Stowell and Dr Gary Deed Newcastle University, Australia.
- "Another indirect connection to infection with coagulase
negative Staphylococcus, has been described. The pattern of muscle
catabolism seen in CFS corresponds to that produced by this organism.
"
-
"Bacterial colonosis (BC) was discussed by Henry Butt (Newcastle
NSW). He had found that patients have multiple gut symptoms with absence
of inflammation apparent in faecal samples. Pain and fatigue tended to
be more severe in those with BC than without."
Research paper presented by Henry Butt (Newcastle NSW) to The
Sydney ME / CFS Clinical and Scientific Conference, December 2001
|

