Cardiac and Vascular and Blood vessel problems. Increased risk of heart attack.
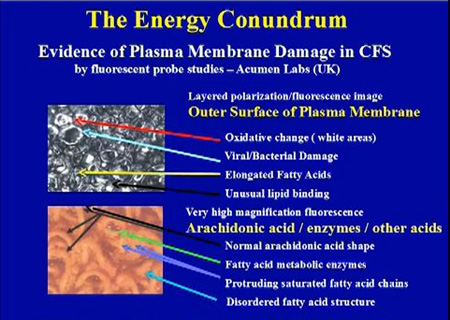
(a)
Abnormal
lipid metabolism. High cholesterol levels
(b) Cardiac Abnormalities & Increased risk of heart attack
(c) Mitral valve prolapse in ME
(d) Raised serum ACE levels
(e) Blood Vessel abnormalities
(f) Hypercoagulablity
(a)
Abnormal lipid metabolism. High cholesterol levels
-
Professor
Peter Behan, The Institute of Neurological Sciences, University of
Glasgow, Scotland.
-
Research
by Professor Anthony Komaroff, Harvard Medical School, USA
-
Bates
DW et al. Arch Intern Med 1995; 155: 97
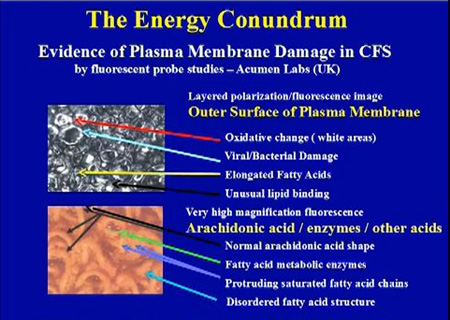
- Increased plasma peroxides as a marker of oxidative stress in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).
Maes M, Kubera M, Uytterhoeven M, Vrydags N, Bosmans E. Med Sci Monit. 2011 Apr;17(4):SC11-5.
(b)
Cardiac Abnormalities & Increased risk of heart attack
Source: ME Primer for Healthcare Professionals: based on Myalgic encephalomyelitis: International Consensus Criteria, 2012
Source: Dr. Paul Cheney, The Cheney Clinic, USA.
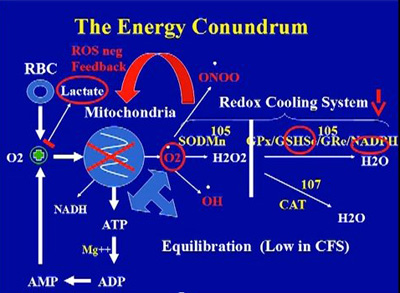
Reduced cardiac fillng, long IVRT, low cardiac output as a
result of mitochondria dysfunctions, infections (some cases),
toxins build up,
and damage caused by high oxidative and nitrosative
stress levels
over time. A very consistent finding in his medical practice.
Dr. Paul Cheney , The Cheney Clinic, USA
Source: Dr. Paul Cheney, The Cheney Clinic, USA
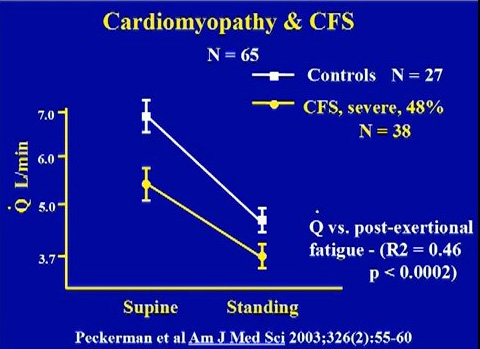
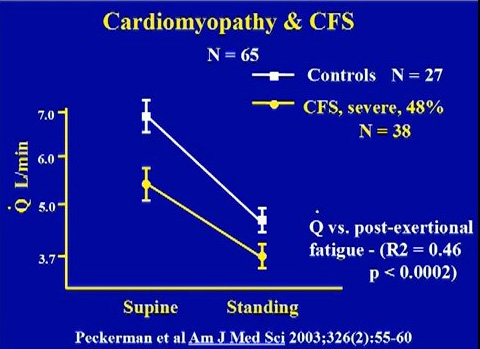
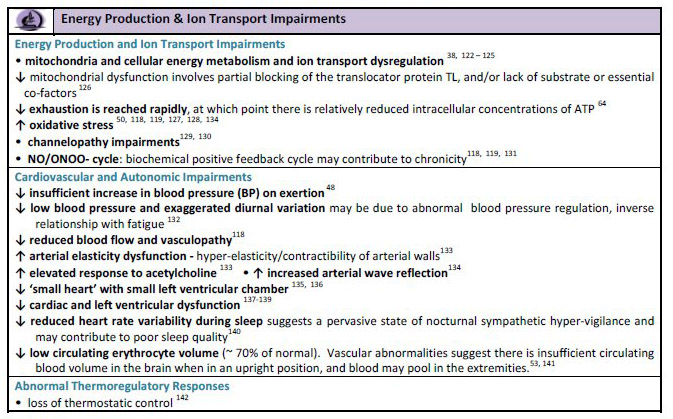
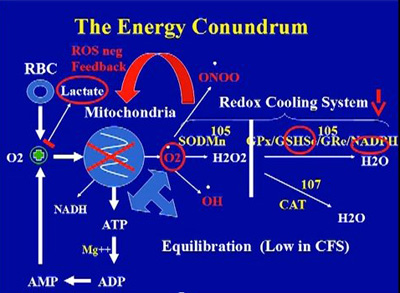
Cardiomyopathy arising from mitochondria dysfunction, oxidative stress and infections
- Peckerman A, et al. Abnormal impedance cardiography predicts symptom severity in chronic fatigue syndrome. Am J Med Sci 2003 Aug;326(2):55-60.
- Peckerman A, LaManca JJ, Qureshi B, et al. 2003 Baroreceptive reflex and integrative stress responses in chronic fatigue syndrome. Psychosom Med 65:889-895.
- Hollingsworth, K. G., Hodgson, T., MacGowan, G. A., Blamire, A. M. and Newton, J. L. (2012), Impaired cardiac function in chronic fatigue syndrome measured using magnetic resonance cardiac tagging. Journal of Internal Medicine, 271: 264–270.
- Elevated nocturnal blood pressure and heart rate in adolescent chronic fatigue syndrome. Harald Hurum, Dag Sulheim, Erik Thaulow, Vegard Bruun Wyller. Acta Paediatrica. Volume 100, Issue 2, pages 289–292, February 2011
.
- Wyller VB, Due R, Saul JP, Amlie JP, Thaulow E. Usefulness of an abnormal
cardiovascular response during low
-
grade head
-
up tilt
-
test for discriminating
adolescents with chronic fatigue
from healthy controls.
Am J Cardiol
(
2007
)
99
:
997
-
1001. doi: 10.1016/j.amjcard.2006.10.067.
- LaManca JJ, Peckerman A, Walker J, Kesil W, Cook S, Taylor A, et al. Cardiovascular
response during head
-
up tilt in chronic fatigue syndrome.
Clin Physiol
(
1999
)
1
9
:
111
-
120. doi: 10.1046/j.1365
-
2281.1999.00154.
- Lerner AM, et al. Repetitively negative T waves at 24-h electrocardiographic monitors in patients
with the Chronic Fatigue Syndrome. Chest 1993, Nov;104(5):1417-142
- Lerner AM, et al. Cardiac involvement in patients with chronic fatigue syndrome as documented
with Holter and biopsy data in Birmingham, Michigan, 1991-1993. Infect Dis Clin
Pract1997;6:327-333
- Codero DL, et al. Decreased vagal power during treadmill walking in patients with chronic
fatigue syndrome. Clin Auton Res 1996 Dec;6(6):329-333
- In ME/CFS, convincing evidence of ca
rdiovascular impairment can be demonstrated".
"Research Update on ME/CFS".
Behan WHM. Professor of Pathology, Glasgow. Extracts from
Over
-
view of the Alison Hunter Memorial Foundation ME/CFS Clinical and Scientific Meeting,
December 2001, Sydney, Austr
alia. For the complete over
-
view, see
http://listserv.nodak.edu/cgi
-
bin/wa.exe?A2=ind0207c&L=co
-
cure&T=0&F=&S=&P=3579
- Rowe PC, Calkins H. Neurally mediated hypotension and chronic fatigue syndrome. Am J Med
1998;105 (3A):15S-21S
- De Becker P, et al. Autonomic testing in patients with chronic fatigue syndrome. Am J of Med
1998; 105(3A):22S-26S
- Schondorf R, Freeman R. The importance of orthostatic intolerance in the chronic fatigue
syndrome. Am J Med Sci 1999;317:117-123
- Hoad A, Spickett G, Elliott J, Newton J.
Postural orthostatic tachycardia syndrome is an under
recognized condition in chronic fatigue syndrome
.
QJM. 2008 Dec;101(12):961-5. Epub 2008
Sep 19.
- Bou-Holaigah I, Rowe PC, Kan J,Calkins H. The relationship between neurally mediated
hypotension and the chronic fatigue syndrome. JAMA. 1995 Sept 27;274(12): 961-967
- Rowe PC, Bou-Holaigah I, Kan JS, Calkins H. Is neurally mediated hypotension an
unrecognised cause of chronic fatigue? Lancet 1995;345:623-624
- Streeten DHP, Bell DS. Circulating blood volume in chronic fatigue syndrome. J CFS 1998;4(1):
3-11
- Newton JL, Sheth A, Shin J, Pairman J, Wilton K, Burt JA
,
Jones DE.
Lower ambulatory blood
pressure in chronic fatigue syndrome.
Psychosom Med.
2009 Apr;71(3):361-5. Epub 2009 Mar
17.
- Hurwitz BE
et al.
Chronic fatigue syndrome: illness severity, sedentary lifestyle, blood volume
and evidence of diminished cardiac function.
Clin Sci (Lond). 2009 Oct
19;118(2):125-35
- Why myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) may kill you: disorders in the inflammatory and oxidative and nitrosative stress (IO&NS) pathways may explain cardiovascular disorders in ME/CFS.Maes M, Twisk FN.Maes Clinics, Wilrijk - Antwerp, Belgium. crc.mh@telenet.be Neuro Endocrinol Lett. 2009;30(6):677-93.
- Excerpt from The Complexities of Diagnosis By Dr. Byron Hyde, Chairman, Nightingale Research Foundation, Chapter 3 in
Handbook of Chronic Fatigue Syndrome. Leonard A. Jason, Patricia A. Fennell, Renée R. Taylor
' Dr. John Richardson from Newcastle upon Tyne has followed ME patients in Durham and
Northumberland counties of the United Kingdom for three to four generations. I am aware of no other
physician in the world with such a historic view of ME patients. He has repeatedly demonstrated that
many ME patients go on to develop structural heart injury. The injury is usually valvular or related to
pericardial effusion, and although most settle down, some do not and may develop myopathy. So I started
to look at the hearts of these patients.
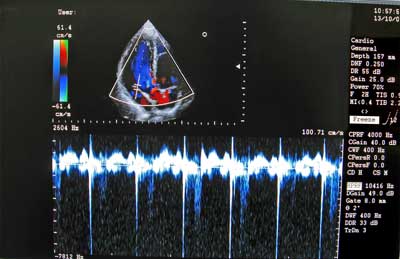
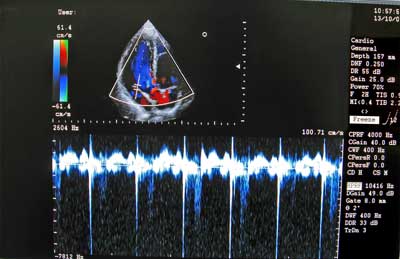
I have found that during the first year of acute onset ME/CFS disability, the incidence of
pericardial effusion is unusually high. This seems to settle down with no apparent short-term problem,
and after a year, the cases of pericardial fluid decrease considerably. However, the incidence of valvular
disease in people in their 30s and 40s appears to be higher than in the normal population. When I find a
significant valvular injury, I then repeat the echocardiogram yearly, and more frequently if the patient
develops shortness of breath. I have observed several cases of elevated right heart pressure, significant
septal defects, and increased myocardial wall thickening. Some who have had the injured valve replaced
have miraculously returned to normal health. Are these incidental findings? I do not know, but Dr.
Richardson has identified more than several hundred cardiopathies in his ME practice. I had two heart
valve replacements in this group in the past year out of a total of 50 new patients.
Carotid and Transcranial Doppler Few physicians investigating ME/CFS employ the visual carotid and transcranial Doppler. This is a major error. It is a relatively inexpensive and totally safe procedure that does things no other type of test can do. On rare occasions, you will find aneurysms and subclavian steal anomaly with this test. Carotid atherosclerosis – sometimes substantial – is often found in
patients with lipid dysfunction. This is a treatable condition and can be part of the cause of a CNS fatigue
syndrome. You may say that any internist or cardiologist can pick up carotid pathology with a stethoscope, but few do who do not have an office Doppler. The carotid scan is also essential if you wish
to do a transcranial Doppler
I examined a patient from the United States who had been diagnosed as having CFS in two major
U.S. CFS clinics. She was given alternative medications and told to return in one year. She had complete
obstruction of the vertebral basilar arteries and approximately 80% and 90% obstruction in either carotid.
I was amazed that she was still alive. She was successfully operated on in Boston and her CFS has
significantly improved.
The transcranial Doppler is not a perfect test. Patients with small foramen magnum space are
difficult to visualize. But it will demonstrate high level internal carotid and other arterial obstruction that
is beyond the normal range of a stethoscope. Only rarely do I get the chance to investigate posttraumatic
mitral valve area (MVA) patients who develop an acute fatigue syndrome where personality or
intellectual change has given rise to the diagnosis of CFS. In two of the past four such patients, I have
demonstrated small subcortical arterial blowouts that had been missed by neurologists and that were
possibly the cause of their pathophysiology.
In patients with ME/CFS, it is possible to demonstrate spasmodic disease of both major and
smaller arteries with no typical evidence of migraine. This arterial pathology may be the end organ
underlying cause of some ME patients' illness. Often MRls and MRAs miss such arterial physiological
pathology. Why? The technology of the MRA consists of a receiving computer revolving around the brain
that may only give a picture of the maximum arterial diameter. In other words, what you see on the MRA
is not reality but one view of reality. With the transcranial Doppler, the operator actually watches and
films the kinetic movement of the arteries within the brain and can measure the velocity of the blood
flow. Not only can you see these arteries move; if they are in spasm, you can observe this as well. Like
ME/CFS muscles, ME brains are sometimes in significant pathological spasm. This knowledge may lead
to more effective treatments of ME/CFS disease. Arterial spasm may account for some, but not all, of the
SPECT changes that are routinely seen in ME patients.
I often find partial or complete vertebral or basilar artery obstruction. Frequently, I find left
middle cerebral artery spasm or obstruction and, less frequently, frontal artery spasm in ME/CFS patients
who do not report a migraine history. Left middle cerebral arterial field hypoperfusion is typical of ME. '
- Prevalence of abnormal cardiac wall motion in the cardiomyopathy associated with incomplete multiplication of Epstein-Barr virus and/or cytomegalovirus in patients with chronic fatigue syndrome. Lerner et al. In Vivo, 18:417-424 (2004)
- Hurwitz BE, Cor
yell VT, Parker M, Martin P, Laperriere A, Klimas NG, et al. Chronic
fatigue syndrome: illness severity, sedentary lifestyle, blood volume and evidence of
diminished cardiac function.
Clin Sci (Lond)
(
2009
)
118
:
125
-
135. doi:
10.1042/CS20090055.
- Hollingswo
rth KG, Hodgson T, Macgowan GA, Blamire AM, Newton JL. Impaired
cardiac function in chronic fatigue syndrome measured using magnetic resonance
cardiac tagging.
J Intern Med
(
2012
)
271
:
264
-
270. doi: 10.1111/j.1365
-
2796.2011.02429.x.
- Miwa K, Fujita M. Cardi
ac function fluctuates during exacerbation and remission in
young adults with chronic fatigue syndrome and "small heart".
J Cardiol
(
2009
)
54
:
29
-
35. doi: 10.1016/j.jjcc.2009.02.008.
- Streeten DH, Bell DS. Circulating blood volume in chronic fatigue syndrom
e.
J Chronic
Fatigue Syndr
(
1998
)
4
:
3
-
11. doi: 10.1300/J092v04n01_02
- Impaired blood pressure variability in chronic fatigue syndrome—a potential biomarker. J. Frith P. Zalewski J. J. Klawe J. Pairman, A. Bitner M. Tafil-Klawe and J. L. Newton (2012)
-
Cardiac
Involvement in Patients with Chronic Fatigue Syndrome as Documented
with Holter and Biopsy Data in Birmingham, Michigan, 1991-1993 A.
Martin Lerner, James Goldstein, Chug-ho Chang, Marcus Zervos, James T.
Fitzgerald, Howard J. Dworkin, Claudine Lawrie-Hoppen, Steven M.
Korotkin, Marc Brodsky, and William O'Neil; Infectious Disease in
Clinical Practice, 1997;6:327-333
-
Montague TJ, Marrie TJ, Klassen GA, Bewick DJ, Horacek BM: Cardiac function at rest and with exercise in the chronic fatigue syndrome. Chest 1989, 95:779-784.
VanNess JM, Snell CR, Stevens SR, Diminished cardiopulmonary capacity during post-exertional malaise in chronic fatigue syndrome. JCFS 2007; 14. 77-85 -
New
Cardiomyopathy: Pilot Study of Intravenous Ganciclovir in a Subset of
the Chronic Fatigue Syndrome; A. Martin Lerner, Marcus Zervos, Howard
J. Dworkin, Chug-ho Chang, James T. Fitzgerald, James Goldstein,
Claudine Lawrie-Hoppen, Barry Franklin, Steven M. Korotkin, Marc
Brodsky, Daniel Walsh, and William O'Neil; Infectious Disease in
Clinical Practice, 1997;6: 110-117
-
Abnormal
left ventricular myocardial dynamics in eleven pts with CFS. Dworkin
HJ, Lawrie C, Bohdiewicz P, Lerner AM; Clinical Nuclear Medicine 1994
Aug;19(8):675-7
- Reduced Cardiac Vagal Modulation Impacts on Cognitive Performance in Chronic Fatigue Syndrome Beaumont A, Burton AR, Lemon J, Bennett BK, Lloyd A, et al. (2012) Reduced Cardiac Vagal Modulation Impacts on Cognitive Performance in Chronic Fatigue Syndrome. PLoS ONE 7(11): e49518. doi:10.1371/journal.pone.0049518
(c)
Mitral valve prolapse in ME
- A
high percentage of CFS patients develop a type of heart murmur called
"mitral valve prolapse." In severe cases, mitral valve
prolapse can cause chest pain, fatigue, heart arrhythmias, typically
causing the heart to beat too fast, or even lead to sudden death
Hyde,
Byron Marshall, Editor; The Clinical and Scientific Basis of Myalgic
Encephalomyelitis/Chronic Fatigue Syndrome; Nightingale Research
Foundation, Ottawa, Ontario, Canada, 1992.
(d) Raised serum ACE levels
-
Serum
ACE levels were also elevated in 80% of patients with CFS as
compared with only 9.4% of control subjects
Lieberman
J, Bell DS. Am J Med 1993; 95: 407
(e) Blood Vessel abnormalities
- Spence V A, Stewart J. Standing up for ME. Biologist 2004. 5165–70.70.
- Kennedy G, Spence V A, Underwood C. et al Increased neutrophil apoptosis in chronic fatigue syndrome. J Clin Pathol 2004. 57891–893.893. [PMC free article] [PubMed
- Kennedy G, Spence V A, McLaren M. et al Oxidative stress levels are raised in chronic fatigue syndrome and are associated with clinical symptoms. Free Radic Biol Med 2005. 39584–589.589. [PubMed]
- Mast cell dysfunctions and abnormalities. This is linked to inflammation, pain, and blood vessel abnormalities. Some research findings listed on this link - http://phoenixrising.me/archives/13083 and at this link http://mastcellmaster.com/research.php . Abnormalities include:
- Tryptase, histamine, heparin blood
- Eosinophilia, basophilia, monocytosis activity
- Serum chromagranin A
- Serum and urinary leukotriene and prostaglandin isoforms
- Urine methylhistamine after exercise
- abnormal levels of neuropeptide Y as this directly affects mast cell functions
- Spence V A, Khan F, Kennedy G. et al Inflammation and arterial stiffness in patients with Chronic Fatigue Syndrome. 8th International IACFS Conference on Chronic Fatigue Syndrome, Fibromyalgia and other related illnesses, Fort Lauderdale, Floride, USA, January, 2007 .
(f)
Hypercoagulablity
-
CFS
patients with active HHV-6 infection were shown by J Brewer
(Phoenix) to have activation of coagulation and are hypercoagulable.
J Brewer (Phoenix) research paper submitted to the AACFS 5th
International Research, Clinical and Patient Conference, 2001
-
Dr
David Berg looked at four measures of clotting and found out that
there was a high rate of abnormalities in CFS patients. Sonoclot was
abnormal in 18/20 (90% of CFSs)
|
|
Abnormal/total
|
|
Sonoclot
rate (speed of clotting)
|
18/20
|
|
Soluble
fibrin monomer (an intermediate fibrinogen molecule produced
by immune activation of coagulation products)
|
14/16
|
|
Fibrinogen
|
9/19
|
|
Platelet
activation score
|
12/20
|
© Dr. David Berg
Dr. Berg goes on to suggest that ¾ of CFS / fibromyalgia patients have
a genetic predisposition to fibrin deposition and local thrombosis in
blood vessels
Source: Diagnosing and treating chronic fatigue syndrome, by Dr.
Sarah Myhill (Wales, UK)
|