Immune System Dysfunctions and Abnormalities
(a) Immune System Overview.
(b) The
presence of Low Molecular Weight RnaseL (LMW RnaseL) and accompanying
STAT1-alpha and p53 deficiencies.
Channelopathy & Disturbance in the way certain ions (mainly sodium and potassium
salts) are transported in and out of cells across the cell membranes
(c) Abnormal
Natural Killer Cell numbers and activity
(d) Shift to Inflammatory TH2 cytokine dominance in ME / CFS patients. Inflammatory Immune Activation and Neuroinflammation (e) B cell abnormalities, Autoimmunity Factors (f) Neuropeptide Dysfunction
(g)
Cleavage of all six insulin-like growth factor binding
proteins (IGFBPs) with a significant proteolytic cleavage of IGFBP-3
(h) HLA abnormalities
(i) Abnormally high or low CD4/CD8 ratio and other T cell abnormalities
(j) Immunoglobulins
(k) Neuro-Immune Model
(l) Immune Complement activity, Endorphins, Monocytes, Weakened immune response, and other Immune system abnormalities
(m) ME outbreaks suggesting immune system abnormalities and role of viruses and other pathogens
(a)
Immune System Overview.
Source: ME Primer for Healthcare Professionals: based on Myalgic encephalomyelitis: International Consensus Criteria, 2012
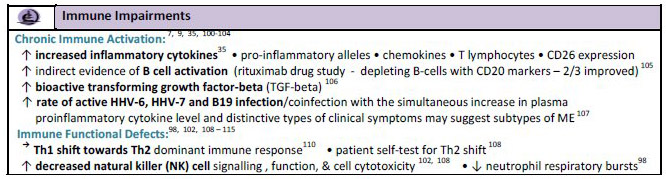
Overview of Immune System markers and associated Genetic markers in ME / CFS
The following video of a lecture by Dr. Gordon Broderick, University of Alberta presents the immune system findings and underlying genes involved in this illness
Dynamic Modeling for ME/CFS & Gulf War Illness Interventions from ME-CFSCommunity.com on Vimeo.
Abnormal Genes and Genetic Pathways
Dr. Gordon Broderick's research team have uncovered several abnormal gene pathways which have direct effects on immune system function, HPA axis function, neurological function and metabolic function. These can differentiate healthy people from those with ME/CFS and also can differentiate ME/CFS from GWS patients.
1. Suppression of alanine and aspartate metabolism (kegg)
2.
Starch and Glucose metabolism (kegg) - increased
3.
Glycolysis / Gluconeogenesis (kegg) - increased
4. Phenylalanine metabolism (kegg) - decreased
5.
Pentose Phosphate pathway (kegg) - increased
6.
Trk (Tyrosine Kinase) receptor signalling mediated by pi3K and plc-gamma (nci/nature) - decreased
7. Disengagement of growth factor signalling and tissue repair ; aurora A
signalling decreased.
Source: Presentation of scientific research findings of Dr. Gordon Broderick
Prefential Pathway Activation in Gulf War Veterans with Unexplained Neuroendocrine Immune Imbalances. G. Broderick et al. (2011)
Overview of defective immune system function during and after infection
Loss of stress response as a consequence of viral infection: implications for disease and therapy.
Hooper PL
,
Hightower LE
,
Hooper PL
Cell Stress Chaperones.
2012 Jul
14. PMID: 22797944
Using an agent-based model to analyze the dynamic communication network of the immune response. Virginia A Folcik, Gordon Broderick, [...], and Clay B Marsh
(b) The
presence of Low Molecular Weight RnaseL (LMW RnaseL) and accompanying
STAT1-alpha and p53 deficiencies and ion channel abnormalities
- Previous studies from this laboratory have demonstrated a statistically significant dysregulation
in several key components of the 2' 5'A synthetase / RNase L and PKR antiviral pathw
ays in
(ME)CFS. The 2
-
5A synthetase
I
RNase L pathway is part of the antiviral defence mechanism in
mammalian cells. An accumulating body of evidence suggests that (ME)CFS is associated with
dysregulation of both humoral and cellular immunity, including mi
togen response, reactivation
of viruses, abnormal cytokine production, diminished natural killer (NK) cell function and
changes in intermediary metabolites. Marked and striking differences have been observed in the
molecular mass and RNase L enzyme activit
y of 2
-
5A binding proteins in extracts of PBMC from
individuals with (ME)CFS compared with healthy controls. The biochemical and immunological
data presented in this paper have identified a potential subgroup of individuals with (ME)CFS
with an RNase L enz
yme dysfunction that is more profound than previously observed in
(ME)CFS, and which the authors believe is related to the severity of (ME)CFS symptoms".
Biochemical Evidence for a Novel Low Molecular Weight 2
-
5A
-
Dependent RNase L in Chronic
Fatigue Synd
rome. Robert J.Suhadolnik Daniel L.Peterson Paul R.Cheney Kenny de Meirleir et al
Journal of Interferon and Cytokine Research 1997:17:377
-
385
- De Meirleir K, et al. A 37 kDa 2-5A binding protein as a potential biochemical marker for chronic fatigue syndrome. Am J Med 2000 Feb;108(2):99-105.
- Nijs J, De Meirleir K: Impairments of the 2-5A synthetase/RNase L pathway in chronic fatigue syndrome. In Vivo 2005, 19:1013-1021.
-
STAT1-alpha
and p53 Deficiencies are Found in Patients with Chronic Fatigue
Syndrome (2003)
Total
Exposure: Expanded Model for RNase L Fragmentation in CFS Uncovered;
The National CFIDS Foundation Announces the Use of Elastase Inhibitors
as a Potential Treatment for CFS Patients (2003)
-
Dr.
Konstance Knox Presents STAT1 Data to Researchers and Clinicians at
AACFS Conference (2004)
-
Potential
Role of STAT1 in the Pathogenesis of Chronic Fatigue Syndrome
Institute, Institute for Viral Pathogenesis (2003)
-
Deficiency in the Expression of STAT1 Protein in a Subpopulation of Patients with Chronic Fatigue Syndrome (CFS); Knox KK, Cocchetto A, Jordan E, Leech D, Carrigan DR; American Association for Chronic Fatigue Syndrome (AACFS) Conference; Madison, Wis; Oct. 2004
-
Biochemical
Evidence for a Novel Low Molecular Weight 2-5A-Dependent RNase L in
Chronic Fatigue Syndrome;
JOURNAL OF INTERFERON AND CYTOKINE RESEARCH 17:377-385 (1997);
Robert I Suhadolnik, Daniel L Peterson, Karen O'Brien, Paul R. Cheney,
C.V.T. Herst, Nancy L. Reichenbach, Ning Kon, Susan E. Horvath,
Kathryn T. Iacono, Martin E. Adelson, Kenny De Meirleir, Pascale De
Becker, Ramamurthy Charubala, and Wolfgang Pfleiderer
- Interactions Between Rnase L Ankyrin-Like Domain and ABC Transporters as a Possible Origin for Pain, Ion Transport, CNS and Immune Disorders of Chronic Fatigue Immune Dysfunction Syndrome. Englebienne et al. 2001.
- Suhadolnik RJ, Peterson D, Reichenbach NL, Roen G, Metzger M, McCahen J, O'Brien K, Welsch S, Gabriel J, Gaughan JP, McGregor NR: Clinical and biochemical characteristics differentiating chronic fatigue syndrome from major depression and healthy control populations: relation to dysfunction and RNase L pathway. J Chron Fatigue Syndr 2004, 12:5-35.
- "This
seriously disrupts the body's immune system and protection against
viruses. Low Molecular Weight RnaseL (LMW RnaseL) is cited as a
possible bio-marker of ME / CFS."
Professor Suhadolnik, Dr. Lebleu (France), Professor Kenny De Meirleir
(Belgium). Research paper submitted to the AACFS 5th International
Research, Clinical and Patient Conference, 2001
- Immunophenotyping predictive of mycoplasma infection in patients with chronic fatigue Syndrome. By J. Nijs et al., J. Chronic Fatigue Syndr. 2003; 11(2): 51-70.
- The 2-5A Pathway and Signal Transduction: A Possible Link to Immune Dysregulation and Fatigue; Englebienne P, Herst CV, Fremont M, Verbinnen T, Verhas M, DeMeirleir K; 5: 99-130; Chronic Fatigue Syndrome: A Biological Approach; CRC Press, 2002
-
'
Changes in the 2-5A Synthetase/Rnase L Antiviral Pathway in a
Controlled Clinical Trial with Poly(I)-Poly(C12U) in Chronic Fatigue
Syndrome '
Roert J. Suhadolnik et al., In Vivo 8 (1994): 599-604.
Thirteen of the 15 people studied had a dramatically increased (upregulated)
level of RNase L enzyme activity, as much as 1,500 times above normal
levels. As their symptoms improved, their RNase L activity returned
towards normal
"Poly(I)-Poly(C12U)" is the molecular name for Ampligen"
Elevated
levels of RnaseL are associated with reduced VO2max and exercise
duration in those with CFS. The low tolerance for exercise may be
linked to abnormal oxidative metabolism. The results have implications
for the testing of antiviral therapies in CFS, particularly those
directed at the 2-5A sythease/ribonuclease L pathway. "
Dr. C. Snell (Philadelphia) research paper submitted to the AACFS 5th
International Research, Clinical and Patient Conference, 2001
Vojdani A
,
Lapp CW
. Interferon-induced proteins are elevated in blood samples of
patients with chemically or virally induced chronic fatigue syndrome. Immunopharmacol
Immunotoxicol. 1999 May;21(2):175-202. PMID: 10319275
Certain toxic chemicals and certain viruses produce
the same kinds of inflammatory effects and defects in 2-5A Synthetase and Protein Kinase RNA
(PKR)). Anti IFN beta inhibited
the reactions.
- Dr. Paul Cheney has successfully treated hundreds of CFS patients in the USA.
Lecture by Dr. Paul Cheney who has successfully treated hundreds of CFS patients in the USA
Summary of the above lecture by Dr. Paul Cheney
-
Normal
NK cell numbers and high LMW / HMW RnaseL ratio correlate with higher
IL-2 levels in CFS patients compared to controls. Dr. Kenny De
Meirleir, research paper submitted to the AACFS 5th International
Research, Clinical and Patient Conference, 2001
-
Structural
and Functional Features of the 37-kDa 2-5A-Dependent RNase L in
Chronic Fatigue Syndrome Journal: J Interferon Cytokine Res 2002
Apr;22(4):443-56
Authors: Shetzline SE, Martinand-Mari C, Reichenbach NL, Buletic Z,
Lebleu B, Pfleiderer W, Charubala R, De Meirleir K, De Becker P,
Peterson DL, Herst CV, Englebienne P, Suhadolnik RJ.
-
Physical
performance and prediction of 2-5A synthetase/RNase L antiviral
pathway activity in patients with chronic fatigue syndrome
ImmuneSupport.com 07-16-2002
Source: In Vivo 2002 Mar-Apr;16(2):107-9 Snell CR, Vanness JM, Strayer
DR, Stevens SR. Department of Sport Sciences, University of the
Pacific, 3601 Pacific Avenue, Stockton, CA 95211-0197, USA
-
Ribonuclease L proteolysis in peripheral blood mononuclear cells of chronic fatigue syndrome patients. J Biol Chem 2002 Jul 12; Demettre E, Bastide L, D'Haese A, De
Smet K, De Meirleir K, Tiev KP, Englebienne P, Lebleu B.
- Chronic Fatigue Syndrome: Exercise Performance Related to Immune Dysfunction. Nijs
et al. 2005
- RNase
L Proteolysis in Chronic Fatigue Syndrome: A Diagnostic Marker ?
By E. Demettre, L. Bastide, A. DĺHaese, K. De Smet, K. De Meirleir,
K. P. Tiev, P. Englebienne and B. Lebleu
These studies were financed by the Centre National de la Recherche
Scientifique, by the CFIDS Association of America and by R.E.D.
Laboratories.
Reported in: ChronicFatigueSyndromeSupport.com
07-31-2002
-
De
Meirleir, K., Bisbal, C., Campine, I., De Becker, P., Salehzada, T.,
Demettre, E., and Lebleu, B. (2000) Am J Med 108(2), 99-105
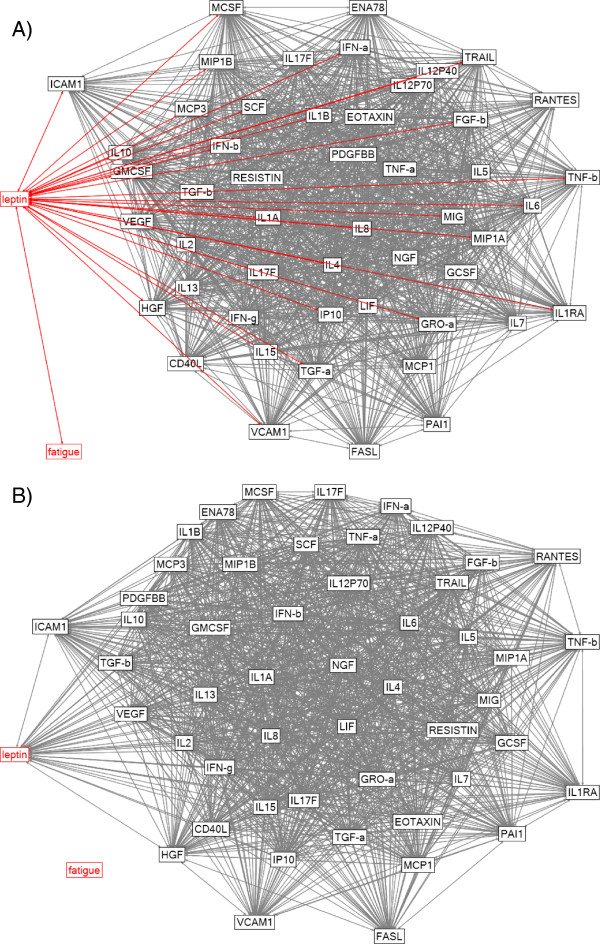
- "Evidence of active HHV6 infection and its correlation with
RNaseL (LMW) protein in CFS patients was presented by Dharam Ablashi
(Washington, USA). His team had looked at HHV6 in plasma, CSF and
white blood cells. The aim was to correlate HHV6 with presence of the
37KDa protein. The 35 CFS patients studied showed that 65% had active
HHV6 infection with varying HHV6 IgM antibody and HHV6 infected PBMCs.
In the CSF, 26.7% had HHV6 DNA. Nested PCR showed 34% patients had
HHV6 in plasma, but using TaqMan PCR, 48.5% were shown positive in
plasma, and 40% in CSF. This test was therefore more sensitive in this
assay. HHV6 variant A was identified by TaqMan PCR in almost all
positive patients. Variant A tends to be acquired in adult life,
variant B in early childhood. Ratio of LMW to HMW(80KDa) protein was
detected in 70% PMBC samples. Correlation with HHV6 was significant
when the ratio was greater than 4. IgM antibody and PCR correlation
was less significant."
Research paper presented by Dharam Ablashi (Washington, USA) to The
Sydney ME / CFS Clinical and Scientific Conference, December 2001
- IMMUNOLOGICAL
ABNORNIALITIES AND THE ANTI-VIRAL Rnase L PATHWAY IN CRONIC FATIGUE
SYNDROME
K.De Meirleir (presenter), I. Campine, P.De Becker, C.V. Herst - Vrije
Universiteit Brussel R. Suhadolnik, N. Reichenbach, S. HoI-vath, D.
Peterson - Temple University, Philadelphia C. Bisbal, T. Salehzada, B.
Lebleu - CNRS Montpellier
Fatigue 2000: International Conference, 23-24 April 1999
- Englebienne P
,
Verhas M
,
Herst CV
,
De Meirleir K
. Type I interferons induce proteins
susceptible to act as thyroid receptor (TR) corepressors and to signal the TR for
destruction by the proteasome: possible etiology for unexplained chronic fatigue.
Med
Hypotheses.
2003 Feb;60(2):175-80. PMID: 12606231
- KIR Receptors
- "Patients indicated significant elevations in the expression of KIR2DL1,
KIR3DL1 and NKG2D compared to the 1994 CDC patients. KIR2DL2
was also significantly higher in ICC patients.
Brenu et al.. Immune Abnormalities in Patients Meeting New Diagnostic Criteria for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis.J Mol Biomark Diagn 2013, 4:3
- Excess of activating killer cell immunoglobulinlike receptors (KIRs) and lack of HLA-Bw4 ligands.
Increased levels of KIR3DS1 and a lack of KIR2DS5 with an absence of HLA-Bw4IIe80 on KIRS3DS1 and KIR3DL1
Pasi, A., Bozzini, S., Carlo-Stella, N., Martinetti, M., Bombardieri, S., De Silvestri, A., Salvaneschi, L. and Cuccia, M., 2011. Excess of activating killer cell immunoglobulinlike receptors and lack of HLA-Bw4 ligands: a twoedged weapon in chronic fatigue syndrome. Molecular medicine reports. 4, 535-40.
- Dr. Sonya Marshall-Gradisnik presented her research teams findings on NK cell and Immunological markers at the International ME Conference 2014. They found a consistent decrease in NK lysis and the severity of the illness reflects the immune changes. There is significant loss of function in KIRs. The dim phenotype KIR2DL1 is significantly reduced, and CD94dim is increased in moderate and severe cases. Dendritic cells are increased significantly in moderate and severe cases. This is accompanied by increased production of cytokines, which cause clinical signs and symptoms. T cell phenotypes are significantly decreased with reduced lysis function. iNKT cells are increased in severe cases and this leads to increased cytokines. NK cell lysis is low and there is significant reduction in adhesion markers. There is decreased migratory ability of NK cells to migrate towards the antigen to lyse.
- "Kenny
de Meirleir and his group looked at the association between
mycoplasmae and the 2-5A/RNaseL pathway in CFS. The hypothesis was
that there maybe a co-morbid physiopathological mechanism between
Mycoplasma infection and the deregulation of the pathway. 182 mainly
female patients, free of antibiotic treatment were enrolled. There was
significant correlation. He showed that mycoplasmae are active in
stimulating some components of the immune system. They can act as
polyclonal T cell and B cell activators. Monocytes produce elastase,
which can cleave 80kDa RNaseL thus causing deregulation of the
antiviral pathway. It has been suggested that LMW RNaseL may reduce
Th1 activity, which implicates susceptibility to infections and a
suppressed ability to eliminate intracellular antigens."
Research paper presented by Kenny de Meirleir (Brussels, Belgium) to
The Sydney ME / CFS Clinical and Scientific Conference, December 2001
-
"P
Englebienne (Brussels) explained how the interaction of RnaseL ankyrin
domain with ABC transporters might explain pain and many of the
physiological disorders of CFS. The study suggests that the possible
dysregulations in ABC transporter function find an origin in their
abnormal interaction with the small fragments of RnaseL containing
ankyrin repeat motifs, released from a proteolytic cleavage of
pathological origin. "
P Englebienne (Brussels) research paper submitted to the AACFS 5th
International Research, Clinical and Patient Conference, 2001
-
As
an accompaniment to the work presented by Englebienne et al several
posters were also displayed clarifying the work of the Belgian team.
The first indicated that the 37kDa LMW RnaseL fragment is produced by
proteolytic cleavage of the native 80kDa monomeric protein. Calpain
has been identified as one of the proteolytic enzymes involved in the
cleavage. The 37kDa fragment could retain both the 2-5a binding and
catalytic activities. S Roelens' posters (Brussels), concluded that in
peripheral blood mononuclear cells (PBMC) in CFS a correlation exists
between the presence of 37kDa binding RnaseL protein and a 26kDa actin
fragment. Some of the actin fragments seen in CFS patients are likely
to be generated by apoptotic proteases. Also the amount of native
actin in the serum correlates with the amount of RnaseL in the PBMC
extracts of CFS patients. A further poster showed that the activation
of RnaseL in the PBMC of CFS patients upregulates apoptotic activity
in these cells, which is likely to be further downregulated by the
large accumulation of its proteolytic cleavage products. This suggests
that accumulation of LMW RnaseL fragments in the PBMC could exert a
blockade in the apoptotic cascade, impairing the elimination of
already damaged cells. RnaseL and G-actin fragments were retrieved in
sorted CD14+cells, which suggests that the perturbed apoptotic process
may play a role in the altered immunologic functioning in CFS.
Report on the AACFS 5th International Research, Clinical and Patient
Conference, 2001
by Dr. Rosamund Vallings
-
"Biochemical
evidence presented by S Shetzline (Brussels) indicates that the origin
of the 37kDa RnaseL in PBMC extracts is more complex than previously
reported as analysis revealed peptide sequences equivalent to human
80kDa RnaseL. "
S Shetzline (Brussels) research paper submitted to the AACFS 5th
International Research, Clinical and Patient Conference, 2001
-
"A
poster also presented by Ablashi et al, showed good concordance
between reactivation of HHV6 and presence of RnaseL. They could
therefore be used together or separately in monitoring response to
treatment. 2 patients were treated with ampligen, which inhibited HHV6
replication and upregulated the 2-5a synthetase/RnaseL pathway."
D Ablashi (Columbia University) research papers submitted to the AACFS
5th International Research, Clinical and Patient Conference, 2001
- Impaired Response to Interferon-Alpha/Beta and Lethal Viral Disease in Human STAT1 Deficiency; Dupuis S, Jouanguy E, Al-Hajjar S, Fieschi C, Al-Mohsen IZ, Al-Jumaah S, Yang K, Chapgier A, Eidenschenk C, Eid P, Al Ghonaium A, Tufenkeji H, Frayha H, Al-Gazlan S, Al-Rayes H, Schreiber RD, Gresser I, Casanova JL; Nat Genet 2003; 33(3): 388-391
- Targeted Disruption of the Mouse STAT1 Gene Results in Compromised Innate Immunity to Viral Disease; Durbin JE, Hackenmiller R, Simon MC, Levy DE; Cell 1996; 84(3): 443-450
- Increased nuclear factor-κB and loss of p53 are key mechanisms in Myalgic Encephalomyelitis/chronic fatigue syndrome (ME/CFS). Morris G, Maes M. Med Hypotheses. 2012 Nov;79(5):607-13.
- Anti-pathogen and immune system treatments. Treatment of 741 italian patients with chronic fatigue syndrome. U. TIRELLI, A. LLESHI, M. BERRETTA, M. SPINA, R. TALAMINI, A. GIACALONE. European Review for Medical and Pharmacological Sciences 2013; 17: 2847-2852
- Hooper M (2007), "Myalgic encephalomyelitis: a review with emphasis on key findings in biomedical research", J Clin Pathol, May;60(5):466-71, Epub 2006 Aug 25,
- "K
de Meirleir (Brussels) found that the presence of an increased amount
of LMW RnaseL correlates with higher levels of IFN gamma, which has
antiviral properties. Normal NK cell numbers and high LMW/HMW RnaseL
ratio correlate with higher IL-2 levels in CFS patients compared to
controls."
K de Meirleir (Brussels) research paper submitted to the AACFS 5th
International Research, Clinical and Patient Conference, 2001
-
"Much
of the Belgian research focused on the abnormal enzyme pathways and
88% of patients tested positive to RnaseL, (as found by Suhadolnik).
The 37Kda is produced by calpain cleavage, and the whole process
affects the calcium and potassium channel mechanisms. RnaseL is a
likely marker for CFS, and correlates with severity. (It is negative
in AIDS). The ALT and the haematocrit are adversely affected by the
abnormal RnaseL ratio and when the ratio is higher the serum calcium
is low, which is consistent with a channelopathy. The channelopathy
will lead to low body potassium because of loss, metabolic alkalosis
and hyperventilation syndrome. Symptoms relating to CVS, abnormal
hormone levels and abnormal exercise response follow. There is a
secondary hypomagnesia, abnormal sodium retention and changed
tryptophan uptake. The latter leads to depression. The CD4/CD8 ratio
correlates with VO2 max. A very complex model was proposed, the
mechanism leading to a Th1/Th2 shift with viral reactivation and
intracellular opportunistic infections. 68.7% patients were infected
with mycoplasma in Belgian studies with a predominance of M.hominis.
Mycoplasma can lead to calpain cleavage. Mycoplasma can invade all
tissues such as monocytes, muscle cells etc. "
K de Meirleir (Brussels), S Shetzline (Brussels), P Englebienne
(Brussels), P de Becker (Brussels), research papers submitted to the
AACFS 5th International Research, Clinical and Patient Conference,
2001
- J.W. Gow, C. Cannon, W.M.H. Behan, P. Herzyk, S. Keir,
G. Riboldi-Tunnicliffe, et al., "Whole-Genome (33,000
genes) Affymetrix DNA Microarray Analysis of Gene
Expression in Chronic Fatigue Syndrome," Paper presented
at the International Conference on Fatigue Science,
Karuizawa, Japan, 2005.
[11] G. Kennedy, V. A. Spence
- Gow
JW, Simpson K, Behan P.O., Chadhuri A, IC and Behan WM. Antiviral
pathway activation in patients with chronic fatigue syndrome and acute
infection. Journal of Infectious Diseases, 2001, 33, online E-CID, 6th
November. (www.journals.uchicago.edu/CID/journal/rapid.html )
- Host response to infection. Including post-infection phase.
Hickie I, et al. Post-infective and chronic fatigue syndromes precipitated by viral and non-viral pathogens: prospective cohort study. British Journal of Medicine 2006; 333 (7568):575.
- Liu et al. Gain-of-function human STAT1 mutations impair IL-17 immunity and underlie chronic mucocutaneous candidiasis, J Exp Med, Aug 1;208(8):1635-48, Epub 2011 Jul 4
- I
have shortly reviewed the 8 abstracts from the AACFS conference in
Seattle dealing with the 37 kDa RNase L. Many of these appear quite
interesting:
1) Abstr. (no 26) Snell et al.: Seventy-eight patients (meeting
CDC-criteria) were studied. Elevated levels of RNase L were associated
with reduced VO2max (oxygen consumption) and exercise duration.
2) Abstr. (no 65) Herst et al.: The37 kDa RNase L fragment is
produced by proteolytic cleavage of the native 80 kDa protein. Calpain
was identified as one of the proteolytic enzymes involved in the
cleavage. The 37 kDa enzyme has retained both its 2-5 A-binding and
catalytic activities thanks to a disulfide bond.
3) Abstr. (no 66) Roelens et al.: In the cell pellets from CFS
patients a correlation exists between the 37 kDa Rnase L and a 26 kDa
actin fragment. Some of the actin are likely generated by apoptotic
proteases.
4) Abstr. (no 67) Roelens et al.: In addition to the above, the
relative percent of the native actin in serum correlates with the
relative percent of the normal RNase L in the cell pellets.
5) Abstr. (no 68) Roelens et al.: The activation of RNase L in
the cell pellets upregulates apoptotic activity in these cells. The
accumulation of LMW RNase L fragments could exert a blockade in the
apoptotic cascade, which could play a role in the altered
immunological functions of CFS.
6) Abstr. (no 69) Herst et al.: The 37 kDa Rnase L contain
ankyrin repeat motifs of the native enzyme. The Rnase L inhibitor (RLI)
take part of the ATP binding cassette (ABC) superfamily and interact
with the ankyrin domain of RNase L. The possible dysregulation in ABC
transporter function find an origin in their abnormal interaction with
small fragments of RNase L containing ankytin repeat motifs, released
from a proteolytic cleavage of pathological origin.
7) Abstr. (no 71) Herst et al.: The two biomarkes 37 kDa RNase
L and reactivation of HHV-6 showed a good concordance in CFS patients,
suggesting their utilization together or separately in monitoring the
patients' response to treatment.
8) Abstr. (no 95) Shetzline et al.: Mass spectrometry analysis
of the 37 kDa RNase L revealed peptide sequences equivalent to the
native 80 kDa, but the kinetic parameters are markedly different. The
origin of the 37 kDa RNase is more complex than previously reported.
RnaseL and PKR can lead to Channelopathy & Disturbance in the way certain ions (mainly sodium and potassium
salts) are transported in and out of cells across the cell membranes
- "Much of the Belgian research focused on the abnormal enzyme pathways and 88% of patients tested positive to RnaseL, (as found by Suhadolnik). The 37Kda is produced by calpain cleavage, and the whole process affects the calcium and potassium channel mechanisms. RnaseL is a likely marker for CFS, and correlates with severity. (It is negative in AIDS). The ALT and the haematocrit are adversely affected by the abnormal RnaseL ratio and when the ratio is higher the serum calcium is low, which is consistent with a channelopathy. The channelopathy will lead to low body potassium because of loss, metabolic alkalosis and hyperventilation syndrome. Symptoms relating to CVS, abnormal hormone levels and abnormal exercise response follow. There is a secondary hypomagnesia, abnormal sodium retention and changed tryptophan uptake. The latter leads to depression. The CD4/CD8 ratio correlates with VO2 max. A very complex model was proposed, the mechanism leading to a Th1/Th2 shift with viral reactivation and intracellular opportunistic infections. 68.7% patients were infected with mycoplasma in Belgian studies with a predominance of M.hominis. Mycoplasma can lead to calpain cleavage. Mycoplasma can invade all tissues such as monocytes, muscle cells etc. "
K de Meirleir (Brussels), S Shetzline (Brussels), P Englebienne (Brussels), P de Becker (Brussels), research papers submitted to the AACFS 5th International Research, Clinical and Patient Conference, 2001
-
“CFS is a poorly-defined medical condition…which, besides severe chronic fatigue as the hallmark symptom, involves inflammatory and immune activation…The type I interferon antiviral pathway has been repeatedly shown to be activated in peripheral blood mononuclear cells of the most severely afflicted patients…Recently, the levels of this abnormal protein have been significantly correlated to the extent of inflammatory symptoms displayed by (ME)CFS patients. We report here that active double-stranded RNA-dependent kinase (PKR) is expressed and activated in parallel to the presence of the 37 kDa RNase L and to an increase in nitric oxide production by immune cells…These results suggest that chronic inflammation due to excess nitric oxide production plays a role in (ME)CFS and that the normal resolution of the inflammatory process by NFK-b activation and apoptotic induction is impaired” (Marc Fremont, Kenny De Meirleir et al. JCFS 2006:13:4:17-28).
- "Pathophysiological mechanisms and CFS were discussed by Kenny de Meirleir (Brussels, Belgium). He described this condition as having no single aetiologic agent, but there are a number of predisposing factors leading to abnormalities in the immune system. Viral reactivation and opportunistic infections increase. Resultant ankyrin fragments from pathologically cleaved RNaseL interact with ABC transporters, which become dysfunctional, leading to many of the symptoms of CFS. This is described as an acquired channelopathy. 206 CFS patients were studied and 70% were found to be Mycoplasma positive, and these patients had significantly more cleavage fragments of RNaseL.
He also mentioned the Bijlmer incident, when following this plane crash, 67% were found to be infected with Mycoplasma, and suffered CFS-like symptoms."
Research findings presented by Professor Kenny de Meirleir (Belgium) to The Sydney ME Clinical and Scientific Conference, December 2001
-
Chronic Fatigue Syndrome is an Acquired Neurological Channelopathy. A Chaudhuri, P Behan. Hum Psychopharmacol Clin Exp 1999:14:7-17
-
Chronic Fatigue Syndrome: is total body potassium important? Burnett RB et al Medical Journal of Australia 1996:164:6:384
- Vojdani A, Ghoneum M, Choppa PC, Magtoto L, Lapp CW (1997) Elevated apoptotic cell population in patients with chronic fatigue syndrome: the pivotal role of protein kinase RNA. J Intern Med 242: 465–478. doi: 10.1111/j.1365-2796.1997.tb00019
-
CHRONIC FATIGUE SYNDROME: ACQUIRED NEUROLOGICAL CHANNELOPATHY
Professor Peter O Behan & Dr Abhijit Chaudhuri
Fatigue 2000: International Conference, 23-24 April 1999
-
Arguments for a role of abnormal ionophore function in Chronic Fatigue Syndrome. A Chaudhuri, WS Watson, PO Behan. Chronic Fatigue Syndrome. ed: Yehuda & Mostofsky pub: Plenum Press, New York, 1997
- "Kenny de Meirleir (Brussels, Belgium) gave an overview of the possible immunological pathways that are disrupted in illnesses such as CFS. He presented data suggesting improper activation of 2-5OAS in monocytes in both CFS and chronic MS. (not however in relapsing/remitting MS) This results in inappropriate activation of RNaseL This process ultimately leads to blockade of RNaseL-mediated apoptosis. A complex series of biochemical/immunological events then follows. Resultant RNA fragments are then capable of either activating or down regulating PKR. A subsequent release of NO at high (CFS) rates or low (MS) rates by lymphocytes leads to effects on ion channel, NK cell function, COX2 activation and glutamine release by activated T cells in the brain. The Belgian results suggest that CFS and chronic MS are extremes of an array of dysfunctions in the 2-5A/RNaseL/PKR pathways"
Research paper presented by Kenny de Meirleir (Brussels, Belgium) to The Sydney ME Clinical and Scientific Conference, December 2001
- Channelopathy
- Whistler T, Jones JF, Unger
ER, Vernon SD.
Exercise responsive genes measured in
peripheral blood of women with chronic fatigue syndrome and matched control
subjects.
BMC Physiol
(
2005
)
5
: 5. doi: 10.1186/1472
-
6793
-
5
-
5.
- Broderick G, Craddock RC, Whistler T, Taylor R, Klimas N, Unger
ER.
Identifying
illness parameters in fatiguing syndromes using classical projection methods.
Pharmacogenomics
(
2006
)
7
:
407
-
419. doi: 10.2217/14622416.7.3.407.
- Watson WS, McCreath GT, Chaudhuri A, Behan PO. Possible cell membrane transport
defect in chro
nic fatigue syndrome?
J Chronic Fatigue Syndr
(
1997
)
3
:
1
-
13. doi:
10.1300/J092v03n03_01.
- Cameron B, Galbraith S, Zhang Y, Davenport T, Vollmer
-
Conna U, Wakefield D, et al.
Gene expression correlates of postinfective fatigue syndrome after infectious
monon
ucleosis.
J Infect Dis
(
2007
)
196
:
56
-
66. doi: 10.1086/518614.
(c)
Abnormal Natural Killer Cell numbers and activity
- This is a new way of identifying immune dysfunctions at the molecular level. Significant reductions in the expression levels of miR-21, in both the NK and CD8(+)T cells in the CFS/ME sufferers. Additionally, the expression of miR-17-5p, miR-10a, miR-103, miR-152, miR-146a, miR-106, miR-223 and miR-191 was significantly decreased in NK cells of CFS/ME patients in comparison to the non-fatigued controls. ( Cytotoxic lymphocyte microRNAs as prospective biomarkers for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis. Brenu EW, Ashton KJ, van Driel M, Staines DR, Peterson D, Atkinson GM, Marshall-Gradisnik SM. J Affect Disord. 2012 Dec 10;141(2-3):261-9.)
- Fletcher MA, Zeng XR, Maher K, Levis S, Hurwitz B, et al. (2010) Biomarkers in Chronic Fatigue Syndrome: Evaluation of Natural Killer Cell Function and Dipeptidyl Peptidase IV/CD26. PLoS ONE 5(5): e10817. doi:10.1371/journal.pone.00108
- Brenu
EW, Hardcastle SL, Atkinson GM, Driel ML, Kreijkamp-Kaspers S, et
al. (2013) Natural killer cells in patients with severe chronic fatigue syndrome.
Autoimmunity Highlights: 1-12.
- Maher
KJ, Klimas NG, Fletcher MA (2005) Chronic fatigue syndrome is
associated with diminished intracellular perforin. Clin Exp Immunol 142: 505-
511.
- Decreased
Natural Killer Cell Activity Is Associated with Severity of Chronic
Fatigue Immune Dysfunction Syndrome
Emmanuel A. Ojo Amaize, Edward J. Conley, and James B. Peter
From Specialty Laboratories, Incorporated, Santa Monica, California
and the Fatigue Clinic of Michigan, Flint, Michigan
- CD69 marker. "The expression of the CD69 activation marker on T cells (CD3+, CD3+CD4+, and CD3+CD8+) and on NK cells (CD45+CD56+) was significantly lower in CFS patients than in healthy subjects. These differences were significant to the extent that a significant diagnostic performance was obtained, i.e. the area under the ROC curve was around 89%. No differences either in the number of leukocytes or in the number or percentage of lymphocytes, i.e. CD3, CD4, CD8 and CD19, could be found between CFS patients and the controls. Patients with CFS show defects in T- and NK cell activation."
Decreased expression of CD69 in chronic fatigue syndrome in relation to inflammatory markers: evidence for a severe disorder in the early activation of T lymphocytes and natural killer cells. Mihaylova I, DeRuyter M, Rummens JL, Bosmans E, Maes M.. Neuro Endocrinol Lett. 2007 Aug;28(4):477-83.
- Whiteside TL, Friberg D: Natural killer cells and natural killer cell activity in chronic fatigue syndrome. Am J Med 1998, 105:27S-34S.
- Zhang C, Zhang J, Tian Z: The regulatory effect of natural killer Cells: do “NK-reg cells” exist? Cell Mol Immunol 2006, 3:241-254.
- MiRNAs
- MicroRNAs hsa-miR-99b, hsa-miR-330, hsa-miR-126 and hsa-miR-30c: Potential Diagnostic Biomarkers in Natural Killer (NK) Cells of Patients with Chronic Fatigue Syndrome (CFS)/ Myalgic Encephalomyelitis (ME). Robert D. Petty , Neil E. McCarthy , Rifca Le Dieu , Jonathan R. Kerr
Published: March 11, 2016DOI: 10.1371/journal.pone.0150904
- This is a new way of identifying immune dysfunctions at the molecular level. Significant reductions in the expression levels of miR-21, in both the NK and CD8(+)T cells in the CFS/ME sufferers. Additionally, the expression of miR-17-5p, miR-10a, miR-103, miR-152, miR-146a, miR-106, miR-223 and miR-191 was significantly decreased in NK cells of CFS/ME patients in comparison to the non-fatigued controls. ( Cytotoxic lymphocyte microRNAs as prospective biomarkers for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis. Brenu EW, Ashton KJ, van Driel M, Staines DR, Peterson D, Atkinson GM, Marshall-Gradisnik SM. J Affect Disord. 2012 Dec 10;141(2-3):261-9.)
- Decreases in several miRNAs - miR-1467a, miR-106b, miR-191, miR-223 increase production of pro-inflammatory molecules
Immunology Primer for Practitioners.
IACFS/ME Conference. Translating Science into Clinical Care. March 20-23, 2014 • San Francisco, California, USA .
- Dr. Sonya Marshall-Gradisnik presented her research teams findings on Immunological markers at the International ME Conference 2014. MiRNA plasma in ME - significant differences are expressed between ME cases and non-fatigued controls.
- Dr. Sonya Marshall-Gradisnik presented her research teams findings on NK cell and Immunological markers at the International ME Conference 2014. NK cell lysis is low and there is significant reduction in adhesion markers. There is decreased migratory ability of NK cells to migrate towards the antigen to lyse. MiRNA plasma in ME - significant differences are expressed between ME cases and non-fatigued controls. There is significant increase in naive B cell phenotypes, specifically memory and naive B cells, due to increased dendritic cell and cytokine production. This indicates an auto-immune response.
- Dr. Sonya Marshall-Gradisnik presented her research teams findings on NK cell and Immunological markers at the International ME Conference 2014. They found a consistent decrease in NK lysis and the severity of the illness reflects the immune changes. There is significant loss of function in KIRs. The dim phenotype KIR2DL1 is significantly reduced, and CD94dim is increased in moderate and severe cases. Dendritic cells are increased significantly in moderate and severe cases. This is accompanied by increased production of cytokines, which cause clinical signs and symptoms. T cell phenotypes are significantly decreased with reduced lysis function. iNKT cells are increased in severe cases and this leads to increased cytokines. NK cell lysis is low and there is significant reduction in adhesion markers. There is decreased migratory ability of NK cells to migrate towards the antigen to lyse. MiRNA plasma in ME - significant differences are expressed between ME cases and non-fatigued controls. There is significant increase in naive B cell phenotypes, specifically memory and naive B cells, due to increased dendritic cell and cytokine production. This indicates an auto-immune response.
- Decreases in several miRNAs - miR-1467a, miR-106b, miR-191, miR-223 increase production of pro-inflammatory molecules
Immunology Primer for Practitioners. IACFS/ME Conference. Translating Science into Clinical Care. March 20-23, 2014 • San Francisco, California, USA
- "low numbers of NKH1+T3- lymphocytes .................When tested for cytotoxicity against a variety of different target cells, patients with CFS consistently demonstrated low levels of killing."
73 percent of ME cases had a decrease in the number of NK cells, and the T3 negative subset was reduced in 50 percent.
Caligiuri
M, Murray C, Buchwald D, et al. Phenotypic and functional deficiency of natural killer cells in patients with chronic fatigue syndrome. J
Immunol 1987:139:3306-13.
- Dr. Sonya Marshall-Gradisnik presented her research teams findings on NK cell and Immunological markers at the International ME Conference 2014. They found a consistent decrease in NK lysis and the severity of the illness reflects the immune changes. There is significant loss of function in KIRs. The dim phenotype KIR2DL1 is significantly reduced, and CD94dim is increased in moderate and severe cases. Dendritic cells are increased significantly in moderate and severe cases. This is accompanied by increased production of cytokines, which cause clinical signs and symptoms. T cell phenotypes are significantly decreased with reduced lysis function. iNKT cells are increased in severe cases and this leads to increased cytokines. NK cell lysis is low and there is significant reduction in adhesion markers. There is decreased migratory ability of NK cells to migrate towards the antigen to lyse. MiRNA plasma in ME - significant differences are expressed between ME cases and non-fatigued controls. There is significant increase in naive B cell phenotypes, specifically memory and naive B cells, due to increased dendritic cell and cytokine production. This indicates an auto-immune response.
- Abnormalities in Granzyme A, B, and perforin are related to NK cell dysfunctions in ME
Natural Killer Cell Degranulation in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis
Teilah K. Huth, Ekua W. Brenu, Kirsty Fuller, Sharni L. Hardcastle, Sam Johnston, Donald R. Staines, Sonya M. Marshall-Gradisnik.
IACFS/ME Conference. Translating Science into Clinical Care. March 20-23, 2014 • San Francisco, California, USA
- "K
Maher found in preliminary studies that the intracellular content of
NK cell lytic protein, perforin, correlates with the cytolytic
potential of the cell. If perforin is removed in mice, the immune
abnormalities are the same as in CFS and also as in a genetic
disease of childhood (FHL) in which there is a mutation in the
perforin gene causing impaired cytotoxic activity. Cytolytic protein
granule protein concentrations were measured in CFS in an attempt to
define the mechanism underlying the reported cytotoxic effects in
CFS. Results showed that intracellular perforin was reduced in NK
cells and in cytotoxic T cells in CFS patients. The findings
substantiate the claims of an NK associated defect in CFS and
suggest a molecular basis for reduced cytotoxicity."
K. Maher et al (Miami) research paper submitted to the AACFS 5th
International Research, Clinical and Patient Conference, 2001.
- Masuda A, Munemoto T, Yamanaka T, et al. Psychosocial characteristics and immunological functions in patients with post infectious chronic fatigue syndrome and non infectious chronic fatigue syndrome.
J Behav Med. 2002; 25:477–85
- NK cell lysis is reduced. Significant reduction in Interferon-gamma in NK bright cells. CD107 degranulation- significant increase, suggesting impaired degranulation.
Immunology Primer for Practitioners.
Natural Killer Cell Subset Distribution of Lytic Proteins in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis
Teilah K. Huth, Ekua W. Brenu, Sharni L. Hardcastle, Kirsty Fuller, Sam Johnston, Donald R. Staines, Sonya M. Marshall-Gradisnik
Natural Killer Cell Degranulation in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis
Teilah K. Huth, Ekua W. Brenu, Kirsty Fuller, Sharni L. Hardcastle, Sam Johnston, Donald R. Staines, Sonya M. Marshall-Gradisnik
IACFS/ME Conference. Translating Science into Clinical Care. March 20-23, 2014 • San Francisco, California, USA
- Abnormalities in Granzyme A, B, and perforin are related to NK cell dysfunctions in ME
Natural Killer Cell Degranulation in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis
Teilah K. Huth, Ekua W. Brenu, Kirsty Fuller, Sharni L. Hardcastle, Sam Johnston, Donald R. Staines, Sonya M. Marshall-Gradisnik.
IACFS/ME Conference. Translating Science into Clinical Care. March 20-23, 2014 • San Francisco, California, USA
- Immunology Primer for Practitioners.
IACFS/ME Conference. Translating Science into Clinical Care. March 20-23, 2014 • San Francisco, California, USA
Daniel Peterson, M.D., Griffith University, Gold Coast, Australia, Owner, Sierra Internal Medicine, Incline Village, NV
Sonya Marshall - Gradisnik, BSc (Hons), Ph.D. , Professor of Immunology, Director, National Centre for Neuroimmunology & Emerging Diseases, Griffith University, Australia
Sharni Hardcastle, Ph.D., Research Assistant and Practical Demonstrator , Bond University, Gold Coast, Australia
Nancy Klimas, M.D. Ph.D., Professor of Medicine and Director, NSU COM Institute for Neuro-Immune Medicine Director, Miami VAMC Gulf War Illness and ME/CFS Research Program
Paula Waziry, Ph.D, Assistant Professor, Neuro Immune Medicine, COM, Nova Southeastern University, Miami, Fl
Konstance Knox, Ph.D., Founder, CEO, Coppe Healthcare Solutions
David Baewer, M.D. Ph.D, Medical Director, Coppe Healthcare Solutions
Isabel Barao, Ph.D., Research Assistant Professor, University of Nevada, Reno, Simmaron Research Scientific
Gunnar Gottschalk, B.S., Simmaron Research, Incline Village, NV
Troy Querec, Ph.D., Associate Service Fellow, Centers for Disease Control and Prevention, Atlanta, GA
Dennis Mangan, Ph.D., Chair, Trans-NIH ME/CFS Research Working Group, Office of Research on Women's Health, U.S. National Institutes of Health
Mary Ann Fletcher, Ph.D., University of Miami Miller School of Medicine Professor of Medicine, Microbiology/Immunology and Psychology
Elizabeth Unger, M.D. Ph.D., Chief, Chronic Viral Disease Branch, Division of High-Consequence Pathogens and Pathology, National Center for Emerging and Zoonotic Infectious Diseases. Centers for Disease Control and Prevention, Atlanta, GA
- Lusso,
Paolo, Mauro S. Mainati, Alfredo Garzino-Demo, Richard W. Crowley,
Eric O. Long, and Robert C. Gallo; "Infection of Natural Killer
Cells by Human Herpesvirus 6"; Nature 862:459, April 1, 1993.
-
The clinical findings of Dr. Edward Conley of the Fatigue, Fibromyalgia and Autoimmune Clinic, Michigan, USA . show that immune system dysfunctions and abnormalities are consistently found in ME / CFS patients and this is detailed in his book America Exhausted: Breakthrough Treatments of Fatigue and Fibromyalgia
-
Immune
activation , as demonstrated by elevation of activated T
lymphocytes, including cytotoxic T cells as well as elevations of
circulating cytokines poor cellular function, with low natural
killer cell cytotoxicity, poor lymphocyte response to mitogens in
culture and frequent immunoglobulin deficiencies, most often IgG1
and IgG3.
R Montero-Petarca, T. Mark, MA Fletcher, N. Klimas. Immunology of
Chronic Fatigue Syndrome. Journal Of Chronic Fatigue Syndrome 2000,
6, 69-107
- Hooper M (2007), "Myalgic encephalomyelitis: a review with emphasis on key findings in biomedical research", J Clin Pathol, May;60(5):466-71, Epub 2006 Aug 25
- The Dubbo Studies which were published in leading medical journals point to genetic factors, environmental factors and a post-infectious dysfunctional immune system as being the key factors in ME / CFS.
Post-infective and chronic fatigue syndromes precipitated by viral and non-viral pathogens: prospective cohort study. Hickie I, Davenport T, Wakefield D, Vollmer-Conna U, Cameron B, Vernon SD, Reeves WC, Lloyd A; Dubbo Infection Outcomes Study Group.
BMJ. 2006 Sep 16;333(7568):575. Epub 2006 Sep 1.
Cytokine polymorphisms have a synergistic effect on severity of the acute sickness response to infection.
Vollmer-Conna U, Piraino BF, Cameron B, Davenport T, Hickie I, Wakefield D, Lloyd AR; Dubbo Infection Outcomes Study Group.
Clin Infect Dis. 2008 Dec 1;47(11):1418-25. doi: 10.1086/592967.
- Hardcastle SL, Brenu EW, Johnston S, Nguyen T, Huth T, Kaur M, et al. Analysis of
the relationship between immune
dysfunction and symptom severity in patients with
Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (CFS/ME).
J Clin Cell Immunol
(
2014
)
5
:
190.
- Ogawa, M., T. Nishiura, M. Yoshimura, Y. Horikawa, H. Yoshida, Y. Okajima, I. Matsumura, Y. Ishikawa, H. Nakao, Y. Tomiyama, Y. Kanayama, Y. Kanakura, and Y. Matsuzawa. 1998. Decreased nitric oxide-mediated natural killer cell activation in chronic fatigue syndrome. Eur. J. Clin. Investig. 28:937-943.
- Findings
and Testimony of Burke A. Cunha, MD., chief, infectious disease
division, Winthrop-University Hospital, Mineola, N.Y., USA.
"But the most consistent lab evidence that we look for are
elevations of coxsackie B-titers and elevations of HHV-6 titers in
combination with the decrease in the percentage of natural killer T
cells," Cunha explained. "If the patient has two or three
of these abnormalities in our study center, then he or she fits the
laboratory criteria for chronic fatigue. Nearly all patients with
crimson crescents have two out of three of these laboratory
abnormalities," he said.
- Klimas N, Koneru AO: Chronic fatigue syndrome: inflammation, immune function, and neuroendocrine interactions. Curr Rheumatol Rep 2007, 9:482-487
- Gupta,
S. and B. Vayavegula; "A Comprehensive Immunological Analysis in
Chronic Fatigue Syndrome"; Scandanavian Journal of Immunology
33:319, 1991
- Anti-pathogen and immune system treatments. Treatment of 741 italian patients with chronic fatigue syndrome. U. TIRELLI, A. LLESHI, M. BERRETTA, M. SPINA, R. TALAMINI, A. GIACALONE. European Review for Medical and Pharmacological Sciences 2013; 17: 2847-2852
- Klimas,
Nancy G., Fernando R. Salvato, Robert Morgan, and Mary Ann Fletcher;
"Immunologic Abnormalities in Chronic Fatigue Syndrome";
Journal of Clinical Microbiology 28(6):1403, June 1990.
-
Murdoch,
J. Campbell; "Cell Mediated Immunity in Patients With Myalgic
Encephalomyelitis Syndrome"; New Zealand Medical Journal, p.
511, August 10, 1988.
-
Buchwald
D: Fibromyalgia and Chronic Fatigue Syndrome: similarities and
differences. Rheum Dis Clin N A 1996; 22:219--243
- Levine, P. H., T. L. Whiteside, D. Friberg, J. Bryant, G. Colclough, and R. B. Herberman. 1998. Dysfunction of natural killer activity in a family with chronic fatigue syndrome. Clin. Immunol. Immunopathol. 88:96-104.
- Kibler R, Lucas DO, Hicks M, et al: Immune function in hronic active Epstein-Barr virus infection. J Clin Immunol 5:46-54, 1985
- Jason LA, Sorenson M, Porter N, Belkairous N (2010), "An Etiological Model for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome", Neuroscience & Medicine, 2011, 2, 14-27, PMID: 21892413
- Ojo-Amaise EA, Conley EJ, Peters JB: Decreased natural killer cell activity is associated with severity of chronic fatigue immune deficiency syndrome. Clin Inf Dis 18:S157-S159, 1994
- See DM, Broumand N, Sahl L, Tilles JG: In vitro effect of echinacea and ginseng on natural killer and antibody-dependent cell cytotoxicity in healthy subjects and chronic fatigue syndrome or acquired immunodeficiency syndrome. Immunopharmacology 35:229-235, 1997
- Masuda, A., S.-I. Nozoe, T. Matsuyama, and H. Tanaka. 1994. Psychobehavioral and immunological characteristics of adult people with chronic fatigue and patients with chronic fatigue syndrome. Psychosom. Med. 56:512-518.
- Tirelli, U., G. Marotta, S. Improta, and A. Pinto. 1994. Immunological abnormalities in patients with chronic fatigue syndrome. Scand. J. Immunol. 40:601-608.
- Host response to infection. Including post-infection phase.
Hickie I, et al. Post-infective and chronic fatigue syndromes precipitated by viral and non-viral pathogens: prospective cohort study. British Journal of Medicine 2006; 333 (7568):575.
- Meeus M, Mistiaen W, Lambrecht L, Nijs J (2009), "Immunological similarities between cancer and chronic fatigue syndrome: the common link to fatigue?", Anticancer Res, Nov;29(11):4717-26, PMID: 20032425,
- Whiteside TL, Friberg D: Natural killer cells and natural killer cell activity in chronic fatigue syndrome. American Journal of Medicine 1998; 105(3A):27S-34S, 1998
- DuBois RE: Gamma globulin therapy for chronic mononucleosis syndrome. AIDS Res Hum Retroviruses 2(1):S191-S195, 1986
- Barker E, Fujimura SF, Fadem MB, Landay AL, Levy JA: Immunologic abnormalities associated with chronic fatigue syndrome. Clin Infect Dis 18(supp 1):S136-S141, 1994
(d)
Shift to Inflammatory TH2 cytokine dominance in ME / CFS patients. Inflammatory Immune Activation and Neuroinflammation
Pro-inflammatory TH2 cytokine dominance in vast majority, and in a small minority of cases TH1 cytokine dominance of the immune system. Profiling individual cytokines and trying to make them diagnostic cannot work for all ME patients due to
(i)
the existence of subgroups
(ii)
the progression of the illness over time in phases: 2 phases, one phase 3 years or less and one phase more than 3 years (Hornig et al. (2013, 2015).
(iii)
if the patient is having active infection(s) including opportunistic infections
(iv)
whether he/she is in remission or in relapse. And if they have mild, moderate or severe ME.
(v)
the patient's genetic weaknesses
(vi) gradual onset ME or rapid onset ?
.
- Phase of illness related Cytokines
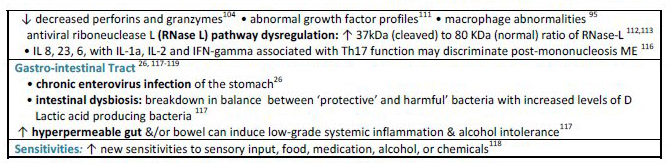
There are significant cytokine differences between patients who have the illness for 3 years or less and those who have it for 3 years or more. The p values in this research are less than 0.05 in many cases, with several less than 0.01, proving that several cytokines are playing an important role in the illness. This is one of the most important findings in recent years. Pro-inflammatory cytokines are increased in the plasma in early phase ME/CFS. Plasma TH2/counter-regulatory cytokines are also increased in early phase ME/CFS. IFNy and IL12p40 are markedly upregulated in early phase ME/CFS. Interferon gamma is quite significant with a p value of .001.
Hornig et al.. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. 27 February 2015, Sci. Adv. 1, e1400121 (2015) DOI: 10.1126/sciadv.1400121
The Chronic Fatigue Initiative (CFI)- Findings from the CFI Cohort Study and Pathogen Discovery & Pathogenesis Project
IACFS/ME Conference. Translating Science into Clinical Care. March 20-23, 2014 • San Francisco, California, USA
- Aspler AL, Bolshin C, Vernon SD, Broderick G (2008), "Evidence of inflammatory immune signaling in chronic fatigue syndrome: A pilot study of gene expression in peripheral blood", Behav Brain Funct, Sep 26;4:44
- Stanford Inflammation Studies. Montoya et al. Stanford University, USA.
IACFS/ME Conference. Translating Science into Clinical Care. March 20-23, 2014 • San Francisco, California, USA
- 197 CFS cases vs. 394 age/sex-matched controls .
- Levels of 51 inflammation-related molecules—cytokine family/chemoknes/hormones measured .
- 15 either distinguished cases from controls, or correlated with symptom severity, or both
Cytokine-by Cytokine Analyses of the Controls, Mild Cases (51-75). Moderate Cases (76-85) and Severe Cases (86-100) and matching this against symptom severity based on MF120. Adjusted for Matched Set
- CGL 11 - 0.00082
- CD40L - 0.00067
- CXCL1 - 0.00653
- CXCL10 - 0.001-42
- GM-CSF - 0.00108
- IFN-7 - 0.00022
- iL-5 - 0.00713
- iL-7 - 0.00265
- iL-12P70 - 0.00615
- iL-13 - 0.00424
- iL-17F - 0.00417
- LEPTIN - 0.00402
- LiF - 0.00702
- RESISTIN - 5e-05
- Raised CCL11 and CXCL10, reduced CSF2, increased levels of Eotaxin (and decreased levels of IL1b) which show an allergic type reaction in the nervous system. These findings suggest an infection of the nervous system and abnormal microglia activation. A strong inflammatory TH2 cytokine response was found in ME patients.
Molecular Psychiatry. 2015 Mar 31. doi: 10.1038/mp.2015.29. [Epub ahead of print] Cytokine network analysis of cerebrospinal fluid in myalgic encephalomyelitis/chronic fatigue syndrome. Hornig M, Gottschalk G, Peterson DL, Knox KK, Schultz AF, Eddy ML, Che X, Lipkin WI
- The Dubbo Studies which were published in leading medical journals point to genetic factors, environmental factors and a post-infectious dysfunctional immune system as being the key factors in ME / CFS.
- Post-infective and chronic fatigue syndromes precipitated by viral and non-viral pathogens: prospective cohort study. Hickie I, Davenport T, Wakefield D, Vollmer-Conna U, Cameron B, Vernon SD, Reeves WC, Lloyd A; Dubbo Infection Outcomes Study Group.
BMJ. 2006 Sep 16;333(7568):575. Epub 2006 Sep 1.
- Cytokine polymorphisms have a synergistic effect on severity of the acute sickness response to infection.
Vollmer-Conna U, Piraino BF, Cameron B, Davenport T, Hickie I, Wakefield D, Lloyd AR; Dubbo Infection Outcomes Study Group.
Clin Infect Dis. 2008 Dec 1;47(11):1418-25. doi: 10.1086/592967.
- Aspler AL, Bolshin C, Vernon SD, Broderick G (2008) Evidence of inflammatory immune signaling in chronic fatigue syndrome: A pilot study of gene expression in peripheral blood. Behav Brain Funct 4: 44
- Phase of illness related Cytokines
There are significant cytokine differences between patients who have the illness for 3 years or less and those who have it for 3 years or more. The p values in this research are less than 0.05 in many cases, with several less than 0.01, proving that several cytokines are playing an important role in the illness. This is one of the most important findings in recent years. Pro-inflammatory cytokines are increased in the plasma in early phase ME/CFS. Plasma TH2/counter-regulatory cytokines are also increased in early phase ME/CFS. IFNy and IL12p40 are markedly upregulated in early phase ME/CFS. Interferon gamma is quite significant with a p value of .001.
Hornig et al.. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. 27 February 2015, Sci. Adv. 1, e1400121 (2015) DOI: 10.1126/sciadv.1400121
The Chronic Fatigue Initiative (CFI)- Findings from the CFI Cohort Study and Pathogen Discovery & Pathogenesis Project
IACFS/ME Conference. Translating Science into Clinical Care. March 20-23, 2014 • San Francisco, California, USA
- IFN alpha and IFN gamma abnormalities
Stimulates macrophages and NK cells to elicit an anti viral response
- Phase of the iIlness : Hornig et al.. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. 27 February 2015, Sci. Adv. 1, e1400121 (2015) DOI: 10.1126/sciadv.1400121
- IACFS/ME Conference. Translating Science into Clinical Care. March 20-23, 2014 • San Francisco, California, USA
- Abnormal levels of IL8, IL6, IL 23, IL1a and IL2, and IFN-gamma associated with Th17 function. Increased inflammatory cytokines (ME Primer for Healthcare Professionals: based on Myalgic encephalomyelitis: International Consensus Criteria, 2012 )
- "Compared to healthy individuals, CFS/ME patients displayed significant increases in IL-10, IFN-γ, TNF-α, CD4+CD25+ T cells, FoxP3 and VPACR2 expression. Cytotoxic activity of NK and CD8+T cells and NK phenotypes, in particular the CD56bright NK cells were significantly decreased in CFS/ME patients. Additionally granzyme A and granzyme K expression were reduced while expression levels of perforin were significantly increased in the CFS/ME population relative to the control population. These data suggest significant dysregulation of the immune system in CFS/ME patients."
Immunological abnormalities as potential biomarkers in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis. Ekua W Brenu, Mieke L van - - Driel, Don R Staines, Kevin J Ashton, Sandra B Ramos, James Keane, Nancy G Klimas, Sonya M Marshall-Gradisnik. Journal of Translational Medicine 2011, 9:81. (2011)
- Innate Immune Changes in the
Peripheral Blood of Chronic Fatigue
Syndrome Patients: Risk Factors for
Disease Progression and Management
Deborah L. S. Goetz, Judy A. Mikovits
, Jamie Deckoff-Jones
and Francis W. Ruscetti,
LANDRES Management Consultant LLC 2
MAR Consulting Inc.
Private CFS Practice. Chronic Fatigue Syndrome. ISBN: 978-1-63321-961-8
- Voll-mer-Conna et al. (2008) found that severe illness following an infection was more likely to occur among individuals with high levels of IFN-γ (a proinflammatory cytokine) and low levels of IL-10 (an anti-inflammatory cytokine)
Vollmer-Conna U, Piraino BF, Cameron B, Davenport T, Hickie I, Wakefield D, Lloyd AR, Dubbo Infection Outcomes Study Group: Cytokine polymorphisms have a synergistic effect on severity of the acute sickness response to infection. Clin Infect Dis 2008, 47:1418-1425.
- Co-expression patterns in 5 cytokines associated with Th17 function may hold promise as a tool for the diagnosis of post-infectious CFS. IL-6, 8 and 23, IL-1a, IL-2 and IFN-γ could be used as a tool for the diagnosis of post-infectious CFS according to scientific paper which tracked patients over 2 years. (Cytokine expression profiles of immune imbalance in post-mononucleosis chronic fatigue. Gordon Broderick, Ben Z Katz, Henrique Fernandes, Mary Ann Fletcher, Nancy Klimas, Frederick A Smith, Maurice RG O'Gorman, Suzanne D Vernon and Renee Taylor. Journal of Translational Medicine 2012, 10:191.)
- abnormal low levels of IFN gamma in Chlamydia infections
- abnormal high levels of IFN alpha in Chronic Lyme infection
- Carlo-Stella N, Badulli C, De Silvestri A, Bazzichi L, Martinetti M, Lorusso L, Bombardieri S, Salvaneschi L, Cuccia M: A first study of cytokine genomic polymorphisms in CFS: positive association of TNF-857 and IFN-gamma 874 rare alleles. Clin Exp Rheumatol 2006, 24:179-182.
- Klimas N, Salvato F, Morgan R, Fletcher MA: Immunologic abnormalities in chronic fatigue syndrome. J Clin Microbiol 28(6):1403-1410, 1990
- Kibler R, Lucas DO, Hicks M, et al: Immune function in hronic active Epstein-Barr virus infection. J Clin Immunol 5:46-54, 1985
- Kerr JR, Barah F, Mattey DL, Laing I, Hopkins SJ, Hutchinson IV, Tyrrell DA: Circulating tumour necrosis factor-alpha and interferon-gamma are detectable during acute and convalescent parvovirus B19 infection and are associated with prolonged and chronic fatigue. J Gen Virol 2001, 82:3011-3019.
- Interferon Poisoning. Dr. Michael Holmes, Dr. Cheney, Dr. Andrew Lloyd
- Visser J, Blauw B, Hinloopen B, Brommer E, de Kloet ER, Kluft C, Nagelkerken L: CD4 T lymphocytes from patients with chronic fatigue syndrome have decreased interferon-gamma production and increased sensitivity to dexamethasone. Journal of Infectious Diseases 177(2):451-454, 1998
- Review: Immunology of Chronic Fatigue Syndrome Roberto Patarca, Timothy Mark, Mary Ann Fletcher and Nancy Klimas Several studies mentioned above confirm this.
- "NK cytotoxic activity was significantly decreased in the CFS/ME patients at T1, T2 and T3 compared to the non-fatigued group. Additionally, in comparison to the non-fatigued controls, the CFS/ME group had significantly lower numbers of CD56 bright CD16 NK cells at both T1 and T2. Interestingly, following mitogenic stimulation, cytokine secretion revealed significant increases in IL-10, IFN-γ and TNF-α at T1 in the CFS/ME group. A significant decrease was observed at T2 in the CFS/ME group for IL-10 and IL-17A while at T3, IL-2 was increased in the CFS/ME group in comparison to the non-fatigued controls. Overall cytotoxic activity was significantly decreased at T3 compared to T1 and T2. CD56bright CD16 NK cells were much lower at T2 compared to T1 and T3. IL-10 and IL-17A secretion was elevated at T2 in comparison to T1 and T3"
"These results confirm decreases in immune function in CFS/ME patients, suggesting an increased susceptibility to viral and other infections. Furthermore, NK cytotoxic activity may be a suitable biomarker for diagnosing CFS/ME as it was consistently decreased during the course of the 12 months study."
Longitudinal investigation of natural killer cells and cytokines in chronic fatigue syndrome/myalgic encephalomyelitis. Ekua W Brenu, Mieke L van Driel, Donald R Staines, Kevin J Ashton, Sharni L Hardcastle, James Keane, Lotti Tajouri, Daniel Peterson, Sandra B Ramos, and Sonya M Marshall-Gradisnik. J Transl Med. 2012; 10 : 88.
- Elevated levels of interferon-gamma (IFN-y). Correlation of IFN-y with cognitive impairment. IFNγ and IL12p40 were significantly increased.
Findings of Chronic Fatigue Initiative, 2014. Immunology Primer for Practitioners.& Chronic Fatigue Initiative Study
IACFS/ME Conference. Translating Science into Clinical Care. March 20-23, 2014 • San Francisco, California, USA
- TNFα and IFNγ were increased in early phase ME/CFS. Eotaxin and CD40L were decreased compared to controls. Findings of Chronic Fatigue Initiative, 2014.
- Vojdani, A., M. Ghoneum, P. C. Choppa, L. Magtoto, and C. W. Lapp. 1997. Elevated apoptotic cell population in patients with chronic fatigue syndrome: the pivotal role of protein kinase RNA. J. Intern. Med. 242:465-478.
- Klimas, N. G., F. R. Salvato, R. Morgan, and M. A. Fletcher. 1990. Immunologic abnormalities in chronic fatigue syndrome. J. Clin. Microbiol. 28:1403-1410.
- Leptin
- Phase of the iIlness : Hornig et al.. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. 27 February 2015, Sci. Adv. 1, e1400121 (2015) DOI: 10.1126/sciadv.1400121
- Upregulation of Leptin in ME patients (Findings of Hornig et al., September 2013).
- Daily cytokine fluctuations, driven by leptin, are associated with fatigue severity in chronic fatigue syndrome: evidence of inflammatory pathology. Elizabeth Ann Stringer, Katharine Susanne Baker, Ian R Carroll, Jose G Montoya, Lily Chu, Holden T Maecker and Jarred W Younger
Journal of Translational Medicine 2013, 11:93
Abnormal Leptin levels are found in several autoimmune illnesses such as autoimmune diabetes, autoimmune thyroid disorders, MS, rheumatoid arthritis and Lupus.
- Abnormal TNF-a levels
Stimulates chronic inflammation
- Phase of the iIlness : Hornig et al.. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. 27 February 2015, Sci. Adv. 1, e1400121 (2015) DOI: 10.1126/sciadv.1400121
- CFS patients have higher levels of sTNF-RI or sCD120a and sTNF-RII or sCD120b (24, 25). Levels of sTNF-Rs are negatively correlated with NK cell cytotoxic and lymphoproliferative activities in CFS, an observation that is consistent with the activities of these soluble mediators. (Review: Immunology of Chronic Fatigue Syndrome Roberto Patarca, Timothy Mark, Mary Ann Fletcher and Nancy Klimas)
- "Compared to healthy individuals, CFS/ME patients displayed significant increases in IL-10, IFN-γ, TNF-α, CD4+CD25+ T cells, FoxP3 and VPACR2 expression. Cytotoxic activity of NK and CD8+T cells and NK phenotypes, in particular the CD56bright NK cells were significantly decreased in CFS/ME patients. Additionally granzyme A and granzyme K expression were reduced while expression levels of perforin were significantly increased in the CFS/ME population relative to the control population. These data suggest significant dysregulation of the immune system in CFS/ME patients."
Immunological abnormalities as potential biomarkers in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis. Ekua W Brenu, Mieke L van Driel, Don R Staines, Kevin J Ashton, Sandra B Ramos, James Keane, Nancy G Klimas, Sonya M Marshall-Gradisnik. Journal of Translational Medicine 2011, 9:81. (2011)
- Raised levels of proinflammatory cytokines, increased levels of interleukin IL 1 and tumor necrosis factor-α, nuclear factor κB, Increased cyclo-oxygenase 2, IL 2, IL 10, transforming growth factor β, osteopontin levels, neopterin, T regulatory (Treg) dysfunction, Forkhead box P3 (FOXP3) dysfunction, Clonal exhaustion of T cells, raised CD26, CD69 expression, activation of immunoinflammatory pathways.
Gerwyn Morris and Michael Maes. Myalgic encephalomyelitis/chronic fatigue syndrome and encephalomyelitis disseminata/multiple sclerosis show remarkable levels of similarity in phenomenology and neuroimmune characteristics. Morris and Maes BMC Medicine 2013 11:205 doi:10.1186/1741-7015-11-205.
- Carlo-Stella N, Badulli C, De Silvestri A, Bazzichi L, Martinetti M, Lorusso L, Bombardieri S, Salvaneschi L, Cuccia M: A first study of cytokine genomic polymorphisms in CFS: positive association of TNF-857 and IFN-gamma 874 rare alleles. Clin Exp Rheumatol 2006, 24:179-182.
- Innate Immune Changes in the
Peripheral Blood of Chronic Fatigue
Syndrome Patients: Risk Factors for
Disease Progression and Management
Deborah L. S. Goetz, Judy A. Mikovits
, Jamie Deckoff-Jones
and Francis W. Ruscetti,
LANDRES Management Consultant LLC 2
MAR Consulting Inc.
Private CFS Practice. Chronic Fatigue Syndrome. ISBN: 978-1-63321-961-8
- Kerr JR, Barah F, Mattey DL, Laing I, Hopkins SJ, Hutchinson IV, Tyrrell DA: Circulating tumour necrosis factor-alpha and interferon-gamma are detectable during acute and convalescent parvovirus B19 infection and are associated with prolonged and chronic fatigue. J Gen Virol 2001, 82:3011-3019.
- also raised in Chlamydia infections
- abnormal high levels in Chronic Lyme infection
- Elevated Serum IL-1, TNFα, neopterin and lysozyme levels. "Serum IL-1, TNFα, neopterin and lysozyme are significantly higher in patients with ME/CFS than in controls" ( Evidence for inflammation and activation of cell-mediated immunity in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): Increased interleukin-1, tumor necrosis factor-α, PMN-elastase, lysozyme and neopterin.
Michael Maes et al. Journal of Affective Disorders Volume 136, Issue 3, February 2012, Pages 933–939 )
- Patarca R, Lugtendorf S, Antoni M, Klimas NG, Fletcher MA: Dysregulated expression of tumor necrosis factor in the chronic fatigue immune dysfunction syndrome: Interrelations with cellular sources and patterns of soluble immune mediator expression. Clinical Infectious Diseases 18:S147-S153, 1994
- Raised levels of proinflammatory cytokines, increased levels of interleukin IL 1 and tumor necrosis factor-α, nuclear factor κB, Increased cyclo-oxygenase 2, IL 2, IL 10, transforming growth factor β, osteopontin levels, neopterin, T regulatory (Treg) dysfunction, Forkhead box P3 (FOXP3) dysfunction, Clonal exhaustion of T cells, raised CD26, CD69 expression, activation of immunoinflammatory pathways.
Gerwyn Morris and Michael Maes. Myalgic encephalomyelitis/chronic fatigue syndrome and encephalomyelitis disseminata/multiple sclerosis show remarkable levels of similarity in phenomenology and neuroimmune characteristics. Morris and Maes BMC Medicine 2013 11:205 doi:10.1186/1741-7015-11-205.
- "NK cytotoxic activity was significantly decreased in the CFS/ME patients at T1, T2 and T3 compared to the non-fatigued group. Additionally, in comparison to the non-fatigued controls, the CFS/ME group had significantly lower numbers of CD56 bright CD16 NK cells at both T1 and T2. Interestingly, following mitogenic stimulation, cytokine secretion revealed significant increases in IL-10, IFN-γ and TNF-α at T1 in the CFS/ME group. A significant decrease was observed at T2 in the CFS/ME group for IL-10 and IL-17A while at T3, IL-2 was increased in the CFS/ME group in comparison to the non-fatigued controls. Overall cytotoxic activity was significantly decreased at T3 compared to T1 and T2. CD56bright CD16 NK cells were much lower at T2 compared to T1 and T3. IL-10 and IL-17A secretion was elevated at T2 in comparison to T1 and T3"
"These results confirm decreases in immune function in CFS/ME patients, suggesting an increased susceptibility to viral and other infections. Furthermore, NK cytotoxic activity may be a suitable biomarker for diagnosing CFS/ME as it was consistently decreased during the course of the 12 months study."
Longitudinal investigation of natural killer cells and cytokines in chronic fatigue syndrome/myalgic encephalomyelitis. Ekua W Brenu, Mieke L van Driel, Donald R Staines, Kevin J Ashton, Sharni L Hardcastle, James Keane, Lotti Tajouri, Daniel Peterson, Sandra B Ramos, and Sonya M Marshall-Gradisnik. J Transl Med. 2012; 10 : 88.
- Decreased IL-17, IL-2, IL-8 and in TNF-alpha in blood plasma. Elevated TH2 cytokines IL-10 and IL-13 and elevated levels of TH1 cytokines IL-1 beta, TNF-alpha, IL-5, and IL-17 in spinal fluid. There are significant differences between patients who have the illness for 3 years or less and those who have it for over 3 years. (Findings of Hornig et al., September 2013)
- Gupta S, Aggarwal S, See D, Starr A: Cytokine production by adherent and non-adherent mononuclear cells in chronic fatigue syndrome. Journal of Psychiatric Research 31(1):149-156, 1997
- Dinarello C: Interleukin-1 and tumor necrosis factor: Effector cytokines in autoimmune diseases. Seminars Immunol 4(3):133-145, 1992
- TNFα and IFNγ were increased in early phase ME/CFS. Eotaxin and CD40L were decreased compared to controls. Findings of Chronic Fatigue Initiative, 2014.
- Borish, L., K. Schmaling, J. D. DiClementi, J. Streib, J. Negri, and J. F. Jones. 1998. Chronic fatigue syndrome: identification of distinct subgroups on the basis of allergy and psychologic variables. J. Allergy Clin. Immunol. 102:222-230.
- Moss, R. B., A. Mercandetti, and A. Vojdani. 1999. TNF-α and chronic fatigue syndrome. J. Clin. Immunol. 19:314-316.
- Patarca, R., N. Klimas, D. Sandler, M. N. Garcia, and M. A. Fletcher. 1996. Interindividual immune status variation patterns in patients with chronic fatigue syndrome: association with gender and the tumor necrosis factor. J. Chronic Fatigue Syndr. 2:13-37.
- Chao, C. C., E. N. Janoff, S. Hu, K. Thomas, M. Gallagher, M. Tsang, and P. K. Peterson. 1991. Altered cytokine release in peripheral blood mononuclear cell cultures from patients with the chronic fatigue syndrome. Cytokine 3:292-298.
- Raised IL-1 and its wider effects
- Phase of the iIlness : Hornig et al.. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. 27 February 2015, Sci. Adv. 1, e1400121 (2015) DOI: 10.1126/sciadv.1400121
- "Standard comparative analysis indicated significant differences in IL-8 and 23 across subject groups. In constructing a linear classification model IL-6, 8 and 23 were selected by two different statistical approaches as discriminating features, with IL-1a, IL-2 and IFN-γ also selected in one model or the other. This supported an assignment accuracy of better than 80% at a confidence level of 0.95 into PI-CFS versus recovered controls."
- Cytokine expression profiles of immune imbalance in post-mononucleosis chronic fatigue. Gordon Broderick, Ben Z Katz,2 Henrique Fernandes, Mary Ann Fletcher, Nancy Klimas, Frederick A Smith, Maurice RG O’Gorman, Suzanne D Vernon, and Renee Taylor. J Transl Med. 2012; 10 : 191.)
- Abnormal levels of IL8, IL6, IL 23, IL1a and IL2, and IFN-gamma associated with Th17 function. Increased inflammatory cytokines (ME Primer for Healthcare Professionals: based on Myalgic encephalomyelitis: International Consensus Criteria, 2012)
- Co-expression patterns in 5 cytokines associated with Th17 function may hold promise as a tool for the diagnosis of post-infectious CFS. IL-6, 8 and 23, IL-1a, IL-2 and IFN-γ could be used as a tool for the diagnosis of post-infectious CFS according to scientific paper which tracked patients over 2 years. (Cytokine expression profiles of immune imbalance in post-mononucleosis chronic fatigue. Gordon Broderick, Ben Z Katz, Henrique Fernandes, Mary Ann Fletcher, Nancy Klimas, Frederick A Smith, Maurice RG O'Gorman, Suzanne D Vernon and Renee Taylor. Journal of Translational Medicine 2012, 10:191.)
- IL-1a also raised in Chlamydia infections
- abnormal high levels of IL1b in Chronic Lyme infection
- Raised levels of proinflammatory cytokines, increased levels of interleukin IL 1 and tumor necrosis factor-α, nuclear factor κB, Increased cyclo-oxygenase 2, IL 2, IL 10, transforming growth factor β, osteopontin levels, neopterin, T regulatory (Treg) dysfunction, Forkhead box P3 (FOXP3) dysfunction, Clonal exhaustion of T cells, raised CD26, CD69 expression, activation of immunoinflammatory pathways.
Gerwyn Morris and Michael Maes. Myalgic encephalomyelitis/chronic fatigue syndrome and encephalomyelitis disseminata/multiple sclerosis show remarkable levels of similarity in phenomenology and neuroimmune characteristics. Morris and Maes BMC Medicine 2013 11:205 doi:10.1186/1741-7015-11-205.
- High levels of Interleukin 1 and 2. Confirmed by Dr. Charles Lapp in one study and by Dr. Cheney and Dr. Bell in another study (5,4).
- Elevated Serum IL-1, TNFα, neopterin and lysozyme levels. "Serum IL-1, TNFα, neopterin and lysozyme are significantly higher in patients with ME/CFS than in controls" ( Evidence for inflammation and activation of cell-mediated immunity in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): Increased interleukin-1, tumor necrosis factor-α, PMN-elastase, lysozyme and neopterin. Michael Maes et al. Journal of Affective Disorders Volume 136, Issue 3, February 2012, Pages 933–939 )
- Linde A, Andersson B, Svenson SB, Ahrne H, Carlsson M, Forsberg P, Hugo H, Karstop A, Lenkei R, Lindwall A, et al: Serum levels of lymphokines and soluble cellular receptors in primary EBV infection and in patients with chronic fatigue syndrome. J Inf Dis 165:994-1000, 1992
- Patarca R, Lugtendorf S, Antoni M, Klimas NG, Fletcher MA: Dysregulated expression of tumor necrosis factor in the chronic fatigue immune dysfunction syndrome: Interrelations with cellular sources and patterns of soluble immune mediator expression. Clinical Infectious Diseases 18:S147-S153, 1994
- Arnason BGW: Nervous system - immune system communication. Rev Infect Dis 13(1):S134-S137, 1991
- Berkenbosch F., J. Van Oers, A. Del Rey, et al: Corticotropin-releasing factor-producing neurons in the RT activated by interleukin-1. Science 238:524-526, 1987
- Decreased IL-17, IL-2, IL-8 and in TNF-alpha in blood plasma. Elevated TH2 cytokines IL-10 and IL-13 and elevated levels of TH1 cytokines IL-1 beta, TNF-alpha, IL-5, and IL-17 in spinal fluid. There are significant differences between patients who have the illness for 3 years or less and those who have it for over 3 years. (Findings of Hornig et al., September 2013)
- Besedovsky H, Del Rey A, Sorkin E, et al: Immunoregulatory feedback between interleukin-1 and glucocorticoid hormones. Science 1986; 233:652-654, 1986
- Sapolsky R, Rivier C, Yamamoto G, et al: Interleukin-1 stimulates the secretion of hypothalamic corticotropin-releasing factor. Science 233:522-524, 1987
- Caverzasio J, Rizzoli R, Dayer JM: Interleukin-1 decreases renal sodium reabsorption: Possible mechanisms of endotoxin-induced natriuresis. Am J Physiol 252:943-6, 1987
- Gulick T, Chung MK, Pieper SJ, et al: Interleukin-1 and tumor necrosis factor inhibit cardiac myocyte beta-adrenergic responsiveness. Proc Natl Acad Sci USA 86:6753-6757, 1989
- Plasma Th2/counter-regulatory cytokines– IL4, IL10, IL13, and IL1RA were increased in patients ill for less than three years. Findings of Chronic Fatigue Initiative, 2014.
- Cannon, J. G., J. B. Angel, L. W. Abad, E. Vannier, M. D. Mileno, L. Fagioli, S. M. Wolff, and A. L. Komaroff. 1997. Interleukin-1β, interleukin-1 receptor antagonist, and soluble interleukin-1 receptor type II secretion in chronic fatigue syndrome. J. Clin. Immunol. 17:253-261.
- Chao, C. C., E. N. Janoff, S. Hu, K. Thomas, M. Gallagher, M. Tsang, and P. K. Peterson. 1991. Altered cytokine release in peripheral blood mononuclear cell cultures from patients with the chronic fatigue syndrome. Cytokine 3:292-298.
- IL 2
- Phase of the iIlness : Hornig et al.. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. 27 February 2015, Sci. Adv. 1, e1400121 (2015) DOI: 10.1126/sciadv.1400121
- Abnormal levels of IL8, IL6, IL 23, IL1a and IL2, and IFN-gamma associated with Th17 function. Increased inflammatory cytokines (ME Primer for Healthcare Professionals: based on Myalgic encephalomyelitis: International Consensus Criteria, 2012 )
- "Standard comparative analysis indicated significant differences in IL-8 and 23 across subject groups. In constructing a linear classification model IL-6, 8 and 23 were selected by two different statistical approaches as discriminating features, with IL-1a, IL-2 and IFN-γ also selected in one model or the other. This supported an assignment accuracy of better than 80% at a confidence level of 0.95 into PI-CFS versus recovered controls."
Cytokine expression profiles of immune imbalance in post-mononucleosis chronic fatigue. Gordon Broderick, Ben Z Katz,2 Henrique Fernandes, Mary Ann Fletcher, Nancy Klimas, Frederick A Smith, Maurice RG O’Gorman, Suzanne D Vernon, and Renee Taylor. J Transl Med. 2012; 10 : 191.)
- Co-expression patterns in 5 cytokines associated with Th17 function may hold promise as a tool for the diagnosis of post-infectious CFS. IL-6, 8 and 23, IL-1a, IL-2 and IFN-γ could be used as a tool for the diagnosis of post-infectious CFS according to scientific paper which tracked patients over 2 years. (Cytokine expression profiles of immune imbalance in post-mononucleosis chronic fatigue. Gordon Broderick, Ben Z Katz, Henrique Fernandes, Mary Ann Fletcher, Nancy Klimas, Frederick A Smith, Maurice RG O'Gorman, Suzanne D Vernon and Renee Taylor. Journal of Translational Medicine 2012, 10:191.)
- Raised levels of proinflammatory cytokines, increased levels of interleukin IL 1 and tumor necrosis factor-α, nuclear factor κB, Increased cyclo-oxygenase 2, IL 2, IL 10, transforming growth factor β, osteopontin levels, neopterin, T regulatory (Treg) dysfunction, Forkhead box P3 (FOXP3) dysfunction, Clonal exhaustion of T cells, raised CD26, CD69 expression, activation of immunoinflammatory pathways.
Gerwyn Morris and Michael Maes. Myalgic encephalomyelitis/chronic fatigue syndrome and encephalomyelitis disseminata/multiple sclerosis show remarkable levels of similarity in phenomenology and neuroimmune characteristics. Morris and Maes BMC Medicine 2013 11:205 doi:10.1186/1741-7015-11-205.
- High levels of Interleukin 1 and 2. Cheney, P. R., S. E. Dorman, and D. S. Bell. 1989. Interleukin-2 and the chronic fatigue syndrome. Ann. Intern. Med. 110:321.
- abnormal high levels in Chronic Lyme infection
- Decreased IL-17, IL-2, IL-8 and in TNF-alpha in blood plasma. Elevated TH2 cytokines IL-10 and IL-13 and elevated levels of TH1 cytokines IL-1 beta, TNF-alpha, IL-5, and IL-17 in spinal fluid. There are significant differences between patients who have the illness for 3 years or less and those who have it for over 3 years. (Findings of Hornig et al., September 2013)
- "NK cytotoxic activity was significantly decreased in the CFS/ME patients at T1, T2 and T3 compared to the non-fatigued group. Additionally, in comparison to the non-fatigued controls, the CFS/ME group had significantly lower numbers of CD56 bright CD16 NK cells at both T1 and T2. Interestingly, following mitogenic stimulation, cytokine secretion revealed significant increases in IL-10, IFN-γ and TNF-α at T1 in the CFS/ME group. A significant decrease was observed at T2 in the CFS/ME group for IL-10 and IL-17A while at T3, IL-2 was increased in the CFS/ME group in comparison to the non-fatigued controls. Overall cytotoxic activity was significantly decreased at T3 compared to T1 and T2. CD56bright CD16 NK cells were much lower at T2 compared to T1 and T3. IL-10 and IL-17A secretion was elevated at T2 in comparison to T1 and T3"
"These results confirm decreases in immune function in CFS/ME patients, suggesting an increased susceptibility to viral and other infections. Furthermore, NK cytotoxic activity may be a suitable biomarker for diagnosing CFS/ME as it was consistently decreased during the course of the 12 months study."
Longitudinal investigation of natural killer cells and cytokines in chronic fatigue syndrome/myalgic encephalomyelitis. Ekua W Brenu, Mieke L van Driel, Donald R Staines, Kevin J Ashton, Sharni L Hardcastle, James Keane, Lotti Tajouri, Daniel Peterson, Sandra B Ramos, and Sonya M Marshall-Gradisnik. J Transl Med. 2012; 10 : 88.
- Rasmussen, ┼. K., H. Nielsen, V. Andersen, T. Barington, K. Bendtzen, M. B. Hansen, L. Nielsen, B. K. Pedersen, and A. Wiik. 1994. Chronic fatigue syndromeŚa controlled cross sectional study. J. Rheumatol. 21:1527-1531.
- IL-4
- Phase of the iIlness : Hornig et al.. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. 27 February 2015, Sci. Adv. 1, e1400121 (2015) DOI: 10.1126/sciadv.1400121
- With CD4 T cells from CFS patients (compared with cells from controls), a 10- to 20-fold lower desamethasone (DEX) concentration was needed to achieve 50% inhibition of IL-4 production and proliferation, indicating an increased sensitivity to DEX in CFS patients. (Review: Immunology of Chronic Fatigue Syndrome Roberto Patarca, Timothy Mark, Mary Ann Fletcher and Nancy Klimas)
- Plasma Th2/counter-regulatory cytokines– IL4, IL10, IL13, and IL1RA were increased in patients ill for less than three years. Findings of Chronic Fatigue Initiative, 2014.
- Increased IL-6
Stimulates chronic inflammation
- Phase of the iIlness : Hornig et al.. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. 27 February 2015, Sci. Adv. 1, e1400121 (2015) DOI: 10.1126/sciadv.1400121
- Abnormal levels of IL8, IL6, IL 23, IL1a and IL2, and IFN-gamma associated with Th17 function. Increased inflammatory cytokines (ME Primer for Healthcare Professionals: based on Myalgic encephalomyelitis: International Consensus Criteria, 2012 )
- CFS patients have higher levels of sIL-6R and sIL-6R enhances the effects of IL-6. This can cause B cell abnormalities and increased risk of autoimmune disease. (Review: Immunology of Chronic Fatigue Syndrome Roberto Patarca, Timothy Mark, Mary Ann Fletcher and Nancy Klimas) Several studies mentioned above confirm this.
- Co-expression patterns in 5 cytokines associated with Th17 function may hold promise as a tool for the diagnosis of post-infectious CFS. IL-6, 8 and 23, IL-1a, IL-2 and IFN-γ could be used as a tool for the diagnosis of post-infectious CFS according to scientific paper which tracked patients over 2 years. (Cytokine expression profiles of immune imbalance in post-mononucleosis chronic fatigue. Gordon Broderick, Ben Z Katz, Henrique Fernandes, Mary Ann Fletcher, Nancy Klimas, Frederick A Smith, Maurice RG O'Gorman, Suzanne D Vernon and Renee Taylor. Journal of Translational Medicine 2012, 10:191.)
- The findings of Dr. Dan Peterson presented at ME/CFS conference, Sweden, 2011.
- also raised in Chlamydia infections
- "Standard comparative analysis indicated significant differences in IL-8 and 23 across subject groups. In constructing a linear classification model IL-6, 8 and 23 were selected by two different statistical approaches as discriminating features, with IL-1a, IL-2 and IFN-γ also selected in one model or the other. This supported an assignment accuracy of better than 80% at a confidence level of 0.95 into PI-CFS versus recovered controls."
- Cytokine expression profiles of immune imbalance in post-mononucleosis chronic fatigue. Gordon Broderick, Ben Z Katz,2 Henrique Fernandes, Mary Ann Fletcher, Nancy Klimas, Frederick A Smith, Maurice RG O’Gorman, Suzanne D Vernon, and Renee Taylor. J Transl Med. 2012; 10 : 191.)
- M. Robinson, S. R. Gray, M.S.Watson, G. Kennedy, A. Hill, J.J. Belch, et al., "Plasma IL-6, its Soluble Receptors and F-Isoprostanes at Rest and During Exercise in Chronic Fatigue Syndrome," Scandinavian Journal of Medicine & Science in Sports, Vol. 13, No. 3,2009, pp. 1-9. doi: 10.1111/j.1600-0838.2009.00895.x
- M. C. Arnold, D. A. Papanicolaou, J. A. O'Grady, A. Lots-ikas, J. K. Dale, S. Straus.,et al., "Using an Interleukin-6 Challenge to Evaluate Neuropsychological Performance in Chronic Fatigue Syndrome. Psychological Medicine, Vol. 32, 2002, pp. 1075-1089
- Gupta, S., S. Aggarwal, D. See, and A. Starr. 1997. Cytokine production by adherent and non-adherent mononuclear cells in chronic fatigue syndrome. J. Psychiatr. Res. 31:149-156.
- Cannon, J. G., J. B. Angel, R. W. Ball, L. W. Abad, L. Fagioli, and A. L. Komaroff. 1999. Acute phase responses and cytokine secretion in chronic fatigue syndrome. J. Clin. Immunol. 19:414-421.
- Chao, C. C., E. N. Janoff, S. Hu, K. Thomas, M. Gallagher, M. Tsang, and P. K. Peterson. 1991. Altered cytokine release in peripheral blood mononuclear cell cultures from patients with the chronic fatigue syndrome. Cytokine 3:292-298.
- Gupta, S., S. Aggarwal, D. See, and A. Starr. 1999. Increased production of interleukin-6 by adherent and non-adherent mononuclear cells during 'natural fatigue' but not following 'experimental fatigue' in patients with chronic fatigue syndrome. Int. J. Mol. Med. 3:209-213
- Buchwald D, Wener MH, Pearlman T, Kith P: Markers of inflammation and immune activation in chronic fatigue and chronic fatigue syndrome. J Rheumatol 1997, 24:372-376.
- Abnormal IL-8
RNaseL and CMV activated
- Phase of the iIlness : Hornig et al.. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. 27 February 2015, Sci. Adv. 1, e1400121 (2015) DOI: 10.1126/sciadv.1400121
- Abnormal levels of IL8, IL6, IL 23, IL1a and IL2, and IFN-gamma associated with Th17 function. Increased inflammatory cytokines (ME Primer for Healthcare Professionals: based on Myalgic encephalomyelitis: International Consensus Criteria, 2012 )
- "Standard comparative analysis indicated significant differences in IL-8 and 23 across subject groups. In constructing a linear classification model IL-6, 8 and 23 were selected by two different statistical approaches as discriminating features, with IL-1a, IL-2 and IFN-γ also selected in one model or the other. This supported an assignment accuracy of better than 80% at a confidence level of 0.95 into PI-CFS versus recovered controls."
Cytokine expression profiles of immune imbalance in post-mononucleosis chronic fatigue. Gordon Broderick, Ben Z Katz,2 Henrique Fernandes, Mary Ann Fletcher, Nancy Klimas, Frederick A Smith, Maurice RG O’Gorman, Suzanne D Vernon, and Renee Taylor. J Transl Med. 2012; 10 : 191.)
- The findings of Dr. Dan Peterson presented at ME/CFS conference, Sweden, 2011.
- also raised in Chlamydia infections
- abnormal high levels in Chronic Lyme disease
- Decreased IL-17, IL-2, IL-8 and in TNF-alpha in blood plasma. Elevated TH2 cytokines IL-10 and IL-13 and elevated levels of TH1 cytokines IL-1 beta, TNF-alpha, IL-5, and IL-17 in spinal fluid. There are significant differences between patients who have the illness for 3 years or less and those who have it for over 3 years. (Findings of Hornig et al., September 2013)
- Innate Immune Changes in the
Peripheral Blood of Chronic Fatigue
Syndrome Patients: Risk Factors for
Disease Progression and Management
Deborah L. S. Goetz, Judy A. Mikovits
, Jamie Deckoff-Jones
and Francis W. Ruscetti,
LANDRES Management Consultant LLC 2
MAR Consulting Inc.
Private CFS Practice. Chronic Fatigue Syndrome. ISBN: 978-1-63321-961-8
- Co-expression patterns in 5 cytokines associated with Th17 function may hold promise as a tool for the diagnosis of post-infectious CFS. IL-6, 8 and 23, IL-1a, IL-2 and IFN-γ could be used as a tool for the diagnosis of post-infectious CFS according to scientific paper which tracked patients over 2 years. (Cytokine expression profiles of immune imbalance in post-mononucleosis chronic fatigue. Gordon Broderick, Ben Z Katz, Henrique Fernandes, Mary Ann Fletcher, Nancy Klimas, Frederick A Smith, Maurice RG O'Gorman, Suzanne D Vernon and Renee Taylor. Journal of Translational Medicine 2012, 10:191.)
- M. Sorenson, N. Porter, L. A. Jason, A. Lerch and H. Matthews, "IL-8 Increased in Patients with CFS," Manuscript Submitted for Publication, 2011.
- MIP1
Elevated in Neurodegenerative disease
- GM-CSF
Stimulates proliferation of B and T lymphocytes and NK cells
- MCP1
Elevated in chronic inflammatory diseases
- Abnormal IL-10
- Phase of the iIlness : Hornig et al.. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. 27 February 2015, Sci. Adv. 1, e1400121 (2015) DOI: 10.1126/sciadv.1400121
"Compared to healthy individuals, CFS/ME patients displayed significant increases in IL-10, IFN-γ, TNF-α, CD4+CD25+ T cells, FoxP3 and VPACR2 expression. Cytotoxic activity of NK and CD8+T cells and NK phenotypes, in particular the CD56bright NK cells were significantly decreased in CFS/ME patients. Additionally granzyme A and granzyme K expression were reduced while expression levels of perforin were significantly increased in the CFS/ME population relative to the control population. These data suggest significant dysregulation of the immune system in CFS/ME patients."
Immunological abnormalities as potential biomarkers in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis. Ekua W Brenu, Mieke L van Driel, Don R Staines, Kevin J Ashton, Sandra B Ramos, James Keane, Nancy G Klimas, Sonya M Marshall-Gradisnik. Journal of Translational Medicine 2011, 9:81. (2011)
- Raised levels of proinflammatory cytokines, increased levels of interleukin IL 1 and tumor necrosis factor-α, nuclear factor κB, Increased cyclo-oxygenase 2, IL 2, IL 10, transforming growth factor β, osteopontin levels, neopterin, T regulatory (Treg) dysfunction, Forkhead box P3 (FOXP3) dysfunction, Clonal exhaustion of T cells, raised CD26, CD69 expression, activation of immunoinflammatory pathways.
Gerwyn Morris and Michael Maes. Myalgic encephalomyelitis/chronic fatigue syndrome and encephalomyelitis disseminata/multiple sclerosis show remarkable levels of similarity in phenomenology and neuroimmune characteristics. Morris and Maes BMC Medicine 2013 11:205 doi:10.1186/1741-7015-11-205.
- abnormal high levels in Chlamydia infections
- abnormal high levels in Chronic Lyme infections
- "NK cytotoxic activity was significantly decreased in the CFS/ME patients at T1, T2 and T3 compared to the non-fatigued group. Additionally, in comparison to the non-fatigued controls, the CFS/ME group had significantly lower numbers of CD56 bright CD16 NK cells at both T1 and T2. Interestingly, following mitogenic stimulation, cytokine secretion revealed significant increases in IL-10, IFN-γ and TNF-α at T1 in the CFS/ME group. A significant decrease was observed at T2 in the CFS/ME group for IL-10 and IL-17A while at T3, IL-2 was increased in the CFS/ME group in comparison to the non-fatigued controls. Overall cytotoxic activity was significantly decreased at T3 compared to T1 and T2. CD56bright CD16 NK cells were much lower at T2 compared to T1 and T3. IL-10 and IL-17A secretion was elevated at T2 in comparison to T1 and T3"
"These results confirm decreases in immune function in CFS/ME patients, suggesting an increased susceptibility to viral and other infections. Furthermore, NK cytotoxic activity may be a suitable biomarker for diagnosing CFS/ME as it was consistently decreased during the course of the 12 months study."
Longitudinal investigation of natural killer cells and cytokines in chronic fatigue syndrome/myalgic encephalomyelitis. Ekua W Brenu, Mieke L van Driel, Donald R Staines, Kevin J Ashton, Sharni L Hardcastle, James Keane, Lotti Tajouri, Daniel Peterson, Sandra B Ramos, and Sonya M Marshall-Gradisnik. J Transl Med. 2012; 10 : 88.
- IACFS/ME Conference. Translating Science into Clinical Care. March 20-23, 2014 • San Francisco, California, USA
- Hornig et al.. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. 27 February 2015, Sci. Adv. 1, e1400121 (2015) DOI: 10.1126/sciadv.1400121
- Innate Immune Changes in the
Peripheral Blood of Chronic Fatigue
Syndrome Patients: Risk Factors for
Disease Progression and Management
Deborah L. S. Goetz, Judy A. Mikovits
, Jamie Deckoff-Jones
and Francis W. Ruscetti,
LANDRES Management Consultant LLC 2
MAR Consulting Inc.
Private CFS Practice. Chronic Fatigue Syndrome. ISBN: 978-1-63321-961-8
- Plasma Th2/counter-regulatory cytokines– IL4, IL10, IL13, and IL1RA were increased in patients ill for less than three years. Findings of Chronic Fatigue Initiative, 2014.
- Visser, J., W. Graffelman, B. Blauw, I. Haspels, E. Lentjes, R. De Kloet, and L. Nagelkerken. 2001. LPS-induced IL-10 production in whole blood cultures from chronic fatigue syndrome patients is increased but supersensitive to inhibition by dexamethasone. J. Neuroimmunol. 119:343-349.
- IL-13
Inhibits inflammatory cytokine production
- Phase of the iIlness : Hornig et al.. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. 27 February 2015, Sci. Adv. 1, e1400121 (2015) DOI: 10.1126/sciadv.1400121
- Decreased IL-17, IL-2, IL-8 and in TNF-alpha in blood plasma. Elevated TH2 cytokines IL-10 and IL-13 and elevated levels of TH1 cytokines IL-1 beta, TNF-alpha, IL-5, and IL-17 in spinal fluid. There are significant differences between patients who have the illness for 3 years or less and those who have it for over 3 years. (Findings of Hornig et al., September 2013)
- Plasma Th2/counter-regulatory cytokines– IL4, IL10, IL13, and IL1RA were increased in patients ill for less than three years. Findings of Chronic Fatigue Initiative, 2014.
- The findings of Dr. Dan Peterson presented at ME/CFS conference, Sweden, 2011.
- IL-17
- Phase of the iIlness : Hornig et al.. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. 27 February 2015, Sci. Adv. 1, e1400121 (2015) DOI: 10.1126/sciadv.1400121
- Decreased IL-17, IL-2, IL-8 and in TNF-alpha in blood plasma. Elevated TH2 cytokines IL-10 and IL-13 and elevated levels of TH1 cytokines IL-1 beta, TNF-alpha, IL-5, and IL-17 in spinal fluid. There are significant differences between patients who have the illness for 3 years or less and those who have it for over 3 years. (Findings of Hornig et al., September 2013)
- "NK cytotoxic activity was significantly decreased in the CFS/ME patients at T1, T2 and T3 compared to the non-fatigued group. Additionally, in comparison to the non-fatigued controls, the CFS/ME group had significantly lower numbers of CD56 bright CD16 NK cells at both T1 and T2. Interestingly, following mitogenic stimulation, cytokine secretion revealed significant increases in IL-10, IFN-γ and TNF-α at T1 in the CFS/ME group. A significant decrease was observed at T2 in the CFS/ME group for IL-10 and IL-17A while at T3, IL-2 was increased in the CFS/ME group in comparison to the non-fatigued controls. Overall cytotoxic activity was significantly decreased at T3 compared to T1 and T2. CD56bright CD16 NK cells were much lower at T2 compared to T1 and T3. IL-10 and IL-17A secretion was elevated at T2 in comparison to T1 and T3"
"These results confirm decreases in immune function in CFS/ME patients, suggesting an increased susceptibility to viral and other infections. Furthermore, NK cytotoxic activity may be a suitable biomarker for diagnosing CFS/ME as it was consistently decreased during the course of the 12 months study."
Longitudinal investigation of natural killer cells and cytokines in chronic fatigue syndrome/myalgic encephalomyelitis. Ekua W Brenu, Mieke L van Driel, Donald R Staines, Kevin J Ashton, Sharni L Hardcastle, James Keane, Lotti Tajouri, Daniel Peterson, Sandra B Ramos, and Sonya M Marshall-Gradisnik. J Transl Med. 2012; 10 : 88.
- Increased IL17 [pro-inflammatory cytokine] and decreased GRO-alpha [a chemokine] are linked to cognitive impairment in ME/CFS.
The Chronic Fatigue Initiative (CFI)- Findings from the CFI Cohort Study and Pathogen Discovery & Pathogenesis Project
IACFS/ME Conference. Translating Science into Clinical Care. March 20-23, 2014 • San Francisco, California, USA
- Elevated levels of IL-17: strongly associated with autoimmunity
Immunology Primer for Practitioners.
IACFS/ME Conference. Translating Science into Clinical Care. March 20-23, 2014 • San Francisco, California, USA
- Abnormal IL-23
- Phase of the iIlness : Hornig et al.. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. 27 February 2015, Sci. Adv. 1, e1400121 (2015) DOI: 10.1126/sciadv.1400121
- Abnormal levels of IL8, IL6, IL 23, IL1a and IL2, and IFN-gamma associated with Th17 function. Increased inflammatory cytokines (ME Primer for Healthcare Professionals: based on Myalgic encephalomyelitis: International Consensus Criteria, 2012 )
- "Standard comparative analysis indicated significant differences in IL-8 and 23 across subject groups. In constructing a linear classification model IL-6, 8 and 23 were selected by two different statistical approaches as discriminating features, with IL-1a, IL-2 and IFN-γ also selected in one model or the other. This supported an assignment accuracy of better than 80% at a confidence level of 0.95 into PI-CFS versus recovered controls."
Cytokine expression profiles of immune imbalance in post-mononucleosis chronic fatigue. Gordon Broderick, Ben Z Katz,2 Henrique Fernandes, Mary Ann Fletcher, Nancy Klimas, Frederick A Smith, Maurice RG O’Gorman, Suzanne D Vernon, and Renee Taylor. J Transl Med. 2012; 10 : 191.)
- Co-expression patterns in 5 cytokines associated with Th17 function may hold promise as a tool for the diagnosis of post-infectious CFS. IL-6, 8 and 23, IL-1a, IL-2 and IFN-γ could be used as a tool for the diagnosis of post-infectious CFS according to scientific paper which tracked patients over 2 years. (Cytokine expression profiles of immune imbalance in post-mononucleosis chronic fatigue. Gordon Broderick, Ben Z Katz, Henrique Fernandes, Mary Ann Fletcher, Nancy Klimas, Frederick A Smith, Maurice RG O'Gorman, Suzanne D Vernon and Renee Taylor. Journal of Translational Medicine 2012, 10:191.)
- Increased TGF-beta levels
- Phase of the iIlness : Hornig et al.. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. 27 February 2015, Sci. Adv. 1, e1400121 (2015) DOI: 10.1126/sciadv.1400121
- Review: Immunology of Chronic Fatigue Syndrome Roberto Patarca, Timothy Mark, Mary Ann Fletcher and Nancy Klimas . Several studies mentioned above confirm this.
- Raised levels of proinflammatory cytokines, increased levels of interleukin IL 1 and tumor necrosis factor-α, nuclear factor κB, Increased cyclo-oxygenase 2, IL 2, IL 10, transforming growth factor β, osteopontin levels, neopterin, T regulatory (Treg) dysfunction, Forkhead box P3 (FOXP3) dysfunction, Clonal exhaustion of T cells, raised CD26, CD69 expression, activation of immunoinflammatory pathways.
Gerwyn Morris and Michael Maes. Myalgic encephalomyelitis/chronic fatigue syndrome and encephalomyelitis disseminata/multiple sclerosis show remarkable levels of similarity in phenomenology and neuroimmune characteristics. Morris and Maes BMC Medicine 2013 11:205 doi:10.1186/1741-7015-11-205.
- also raised in Chlamydia infections
- Bennett, A. L., C. C. Chao, S. Hu, B. Buchwald, L. R. Fagioli, P. H. Schur, P. K. Peterson, and A. L. Komaroff. 1997. Elevation of bioactive transforming growth factor-▀ in serum from patients with chronic fatigue syndrome. J. Clin. Immunol. 17:160-166.
- Allergy related Cytokines
- Phase of the iIlness : Hornig et al.. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. 27 February 2015, Sci. Adv. 1, e1400121 (2015) DOI: 10.1126/sciadv.1400121
- Elevated levels of allergy-associated cytokines and chemokines (IL-4, IL-6, IL-10, IL-13, IL-17A, CCL5) and other pro-inflammatory cytokines (IL-1a, IL1B, IL1-RA, IL-8, MCP1, CXCL-10, MIP1a, IL-12p40, TGFa) in patients ill for < 3 years vs. ill for > 3 years. Eotaxin is decreased in early ME/CFS (ME/CFS less than 3 years).
Allergy-Related Immune Signatures and Duration of Illness in CFS. Susan Levine, Xiaoyu Che, W. Ian Lipkin, Nancy Klimas, Lucinda Bateman, Dan Peterson, Donna Felsenstein, Elizabeth Balbin, Aundrea Carter, Korinne Chu, Mary Ann Fletcher, Anthony Komaroff, Gail Ironson and Mady Hornig
IACFS/ME Conference. Translating Science into Clinical Care. March 20-23, 2014 • San Francisco, California, USA
- Post Exercise Cytokines
- Il1-RA, IL-8, MCP-1 (CCL2) were significantly lower in CFS after one CPET. IL1-RA went down more on day 2 for CFS, and up in controls. Strong indication of immune system dysregulation.
Plasma Cytokines in ME/CFS Patients and Controls Before and After a Cardiopulmonary Exercise Test. Ludovic Giloteaux, Betsy A. Keller, and Maureen R. Hanson. IACFS/ME Conference. Translating Science into Clinical Care. March 20-23, 2014 • San Francisco, California, USA
- Increased beta-2 microglobulin & C-reactive protein
- Buchwald D, Wener MH, Pearlman T, Kith P: Markers of inflammation and immune activation in chronic fatigue and chronic fatigue syndrome. Journal of Rheumatology 24(2):372-6, 1997
- Patarca R, Klimas NG, Garcia MN, Pons H, Fletcher MA: Dysregulated expression of soluble immune mediator receptors in a subset of patients with chronic fatigue syndrome: Categorization of patients by immune status. Journal of Chronic Fatigue Syndrome 1:79-94, 1995
Patarca R, Klimas NG, Sandler D, Garcia MN, Fletcher MA: Interindividual immune status variation patterns in patients with chronic fatigue syndrome: association with the tumor necrosis factor system and gender. Journal of Chronic Fatigue Syndrome 2(1):13-19, 1995
- Buchwald D, Wener MH, Pearlman T, Kith P: Markers of inflammation and immune activation in chronic fatigue and chronic fatigue syndrome. J Rheumatol 1997, 24:372-376.
- Elevated levels of Neopterin in blood and nervous system
- Phase of the iIlness : Hornig et al.. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. 27 February 2015, Sci. Adv. 1, e1400121 (2015) DOI: 10.1126/sciadv.1400121
- Review: Immunology of Chronic Fatigue Syndrome Roberto Patarca, Timothy Mark, Mary Ann Fletcher and Nancy Klimas . Several studies mentioned above confirm this. Also neopterin levels have been shown to correlate with levels of many other mediators that have been found to be dysregulated in CFS including members of the TNF family. Measure levels of neopterin, indoleamine 2,3-dioxygenase, L-kynurenine, kynurenic acid and quinolinic acid in blood, spinal fluids and nerve tissues. Also measure levels of tryptophan. Test for brain lesions consistent with edema, inflammatory destruction and demyelination.
- Elevated Serum IL-1, TNFα, neopterin and lysozyme levels. "Serum IL-1, TNFα, neopterin and lysozyme are significantly higher in patients with ME/CFS than in controls" ( Evidence for inflammation and activation of cell-mediated immunity in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): Increased interleukin-1, tumor necrosis factor-α, PMN-elastase, lysozyme and neopterin.
Michael Maes et al. Journal of Affective Disorders Volume 136, Issue 3, February 2012, Pages 933–939 )
- Raised levels of proinflammatory cytokines, increased levels of interleukin IL 1 and tumor necrosis factor-α, nuclear factor κB, Increased cyclo-oxygenase 2, IL 2, IL 10, transforming growth factor β, osteopontin levels, neopterin, T regulatory (Treg) dysfunction, Forkhead box P3 (FOXP3) dysfunction, Clonal exhaustion of T cells, raised CD26, CD69 expression, activation of immunoinflammatory pathways.
Gerwyn Morris and Michael Maes. Myalgic encephalomyelitis/chronic fatigue syndrome and encephalomyelitis disseminata/multiple sclerosis show remarkable levels of similarity in phenomenology and neuroimmune characteristics. Morris and Maes BMC Medicine 2013 11:205 doi:10.1186/1741-7015-11-205.
- Chao, C. C., M. Gallagher, J. Phair, and P. K. Peterson. 1990. Serum neopterin and interleukin-6 levels in chronic fatigue syndrome. J. Infect. Dis. 162:1412-1413.
- Buchwald D, Wener MH, Pearlman T, Kith P: Markers of inflammation and immune activation in chronic fatigue and chronic fatigue syndrome. J Rheumatol 1997, 24:372-376.
- FoxP3
- Phase of the iIlness : Hornig et al.. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. 27 February 2015, Sci. Adv. 1, e1400121 (2015) DOI: 10.1126/sciadv.1400121
- "Compared to healthy individuals, CFS/ME patients displayed significant increases in IL-10, IFN-γ, TNF-α, CD4+CD25+ T cells, FoxP3 and VPACR2 expression. Cytotoxic activity of NK and CD8+T cells and NK phenotypes, in particular the CD56bright NK cells were significantly decreased in CFS/ME patients. Additionally granzyme A and granzyme K expression were reduced while expression levels of perforin were significantly increased in the CFS/ME population relative to the control population. These data suggest significant dysregulation of the immune system in CFS/ME patients."
Immunological abnormalities as potential biomarkers in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis. Ekua W Brenu, Mieke L van Driel, Don R Staines, Kevin J Ashton, Sandra B Ramos, James Keane, Nancy G Klimas, Sonya M Marshall-Gradisnik. Journal of Translational Medicine 2011, 9:81. (2011)
- Raised levels of proinflammatory cytokines, increased levels of interleukin IL 1 and tumor necrosis factor-α, nuclear factor κB, Increased cyclo-oxygenase 2, IL 2, IL 10, transforming growth factor β, osteopontin levels, neopterin, T regulatory (Treg) dysfunction, Forkhead box P3 (FOXP3) dysfunction, Clonal exhaustion of T cells, raised CD26, CD69 expression, activation of immunoinflammatory pathways.
Gerwyn Morris and Michael Maes. Myalgic encephalomyelitis/chronic fatigue syndrome and encephalomyelitis disseminata/multiple sclerosis show remarkable levels of similarity in phenomenology and neuroimmune characteristics. Morris and Maes BMC Medicine 2013 11:205 doi:10.1186/1741-7015-11-205.
- FOXP3 Upregulation. Invest in ME Scientific Conference 2012, 2013.
- VPACR2 expression.
- Phase of the iIlness : Hornig et al.. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. 27 February 2015, Sci. Adv. 1, e1400121 (2015) DOI: 10.1126/sciadv.1400121
- "Compared to healthy individuals, CFS/ME patients displayed significant increases in IL-10, IFN-γ, TNF-α, CD4+CD25+ T cells, FoxP3 and VPACR2 expression. Cytotoxic activity of NK and CD8+T cells and NK phenotypes, in particular the CD56bright NK cells were significantly decreased in CFS/ME patients. Additionally granzyme A and granzyme K expression were reduced while expression levels of perforin were significantly increased in the CFS/ME population relative to the control population. These data suggest significant dysregulation of the immune system in CFS/ME patients."
Immunological abnormalities as potential biomarkers in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis. Ekua W Brenu, Mieke L van Driel, Don R Staines, Kevin J Ashton, Sandra B Ramos, James Keane, Nancy G Klimas, Sonya M Marshall-Gradisnik. Journal of Translational Medicine 2011, 9:81. (2011)
- Cyclo-oxygenase-2 (COX2), Inducible NO synthase, NFκB
- Phase of the iIlness : Hornig et al.. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. 27 February 2015, Sci. Adv. 1, e1400121 (2015) DOI: 10.1126/sciadv.1400121
- Increased production of cyclo-oxygenase-2 (COX2) and inducible NO synthase and NFκB
Maes M, Mihaylova I, Kubera M, Bosmans E: Not in the mind but in the cell: increased production of cyclo-oxygenase-2 and inducible NO synthase in chronic fatigue syndrome. Neuro Endocrinol Lett 2007, 28:463-469.
- Raised levels of proinflammatory cytokines, increased levels of interleukin IL 1 and tumor necrosis factor-α, nuclear factor κB, Increased cyclo-oxygenase 2, IL 2, IL 10, transforming growth factor β, osteopontin levels, neopterin, T regulatory (Treg) dysfunction, Forkhead box P3 (FOXP3) dysfunction, Clonal exhaustion of T cells, raised CD26, CD69 expression, activation of immunoinflammatory pathways.
Gerwyn Morris and Michael Maes. Myalgic encephalomyelitis/chronic fatigue syndrome and encephalomyelitis disseminata/multiple sclerosis show remarkable levels of similarity in phenomenology and neuroimmune characteristics. Morris and Maes BMC Medicine 2013 11:205 doi:10.1186/1741-7015-11-205.
- also raised in Chronic Lyme disease
- miRNAs
- Decreases in several miRNAs - miR-1467a, miR-106b, miR-191, miR-223 increase production of pro-inflammatory molecules
Immunology Primer for Practitioners. IACFS/ME Conference. Translating Science into Clinical Care. March 20-23, 2014 • San Francisco, California, USA
- MicroRNAs hsa-miR-99b, hsa-miR-330, hsa-miR-126 and hsa-miR-30c: Potential Diagnostic Biomarkers in Natural Killer (NK) Cells of Patients with Chronic Fatigue Syndrome (CFS)/ Myalgic Encephalomyelitis (ME). Robert D. Petty , Neil E. McCarthy , Rifca Le Dieu , Jonathan R. Kerr
Published: March 11, 2016DOI: 10.1371/journal.pone.0150904
- Dr. Sonya Marshall-Gradisnik presented her research teams findings on NK cell and Immunological markers at the International ME Conference 2014. NK cell lysis is low and there is significant reduction in adhesion markers. There is decreased migratory ability of NK cells to migrate towards the antigen to lyse. MiRNA plasma in ME - significant differences are expressed between ME cases and non-fatigued controls. There is significant increase in naive B cell phenotypes, specifically memory and naive B cells, due to increased dendritic cell and cytokine production. This indicates an auto-immune response.
- Dr. Sonya Marshall-Gradisnik presented her research teams findings on NK cell and Immunological markers at the International ME Conference 2014. They found a consistent decrease in NK lysis and the severity of the illness reflects the immune changes. There is significant loss of function in KIRs. The dim phenotype KIR2DL1 is significantly reduced, and CD94dim is increased in moderate and severe cases. Dendritic cells are increased significantly in moderate and severe cases. This is accompanied by increased production of cytokines, which cause clinical signs and symptoms. T cell phenotypes are significantly decreased with reduced lysis function. iNKT cells are increased in severe cases and this leads to increased cytokines. NK cell lysis is low and there is significant reduction in adhesion markers. There is decreased migratory ability of NK cells to migrate towards the antigen to lyse. MiRNA plasma in ME - significant differences are expressed between ME cases and non-fatigued controls. There is significant increase in naive B cell phenotypes, specifically memory and naive B cells, due to increased dendritic cell and cytokine production. This indicates an auto-immune response.
- Dr. Sonya Marshall-Gradisnik presented her research teams findings on NK cell and Immunological markers at the International ME Conference 2014. They found a consistent decrease in NK lysis and the severity of the illness reflects the immune changes. There is significant loss of function in KIRs. The dim phenotype KIR2DL1 is significantly reduced, and CD94dim is increased in moderate and severe cases. Dendritic cells are increased significantly in moderate and severe cases. This is accompanied by increased production of cytokines, which cause clinical signs and symptoms. T cell phenotypes are significantly decreased with reduced lysis function. iNKT cells are increased in severe cases and this leads to increased cytokines. NK cell lysis is low and there is significant reduction in adhesion markers. There is decreased migratory ability of NK cells to migrate towards the antigen to lyse. MiRNA plasma in ME - significant differences are expressed between ME cases and non-fatigued controls. There is significant increase in naive B cell phenotypes, specifically memory and naive B cells, due to increased dendritic cell and cytokine production. This indicates an auto-immune response.
- Host response to infection. Including post-infection phase.
- Hickie I, et al. Post-infective and chronic fatigue syndromes precipitated by viral and non-viral pathogens: prospective cohort study. British Journal of Medicine 2006; 333 (7568):575.
- Voll-mer-Conna et al. (2008) found that severe illness following an infection was more likely to occur among individuals with high levels of IFN-γ (a proinflammatory cytokine) and low levels of IL-10 (an anti-inflammatory cytokine)
Vollmer-Conna U, Piraino BF, Cameron B, Davenport T, Hickie I, Wakefield D, Lloyd AR, Dubbo Infection Outcomes Study Group: Cytokine polymorphisms have a synergistic effect on severity of the acute sickness response to infection. Clin Infect Dis 2008, 47:1418-1425.
- U. Vollmer-Conna, C. Fazou, B. Cameron, H. Li, C. Brennan, L. Luck, et al., "Production of Pro-Inflammatory Cytokines Correlates with Symptoms of Acute Sickness Behaviour in Humans," Psychological Medicine, Vol. 34, 2004, pp. 1-9.
- Cytokine co-expression networks
Cytokine co-expression networks were constructed from the pair-wise mutual information (MI) patterns found within each subject group. Networks for HC and CFS had visibly different topologies (geometric arrangements). A weighted spring-electrical embedding structurally reveals the subject-subject (inset) and cytokine-cytokine associations based on measurements in 59 healthy control subjects (A) and 40 CFS patients (B). All edge weights are significant at p≤0.01. Separation of subjects was consistent with their assignment to diagnostic groups supporting the use of within-group variation in the estimation of mutual information for cytokine-cytokine associations (73). Diagram used with permission.
Broderick G, Fuite J, Kreitz A, Vernonb SD, Klimas N, Fletcherd MA. A Formal Analysis of Cytokine Networks in Chronic Fatigue Syndrome. Brain Behav Immun 2010;24(7): 1209–1217. doi:10.1016/j.bbi.2010.04.012.

- Plasma cytokines in women with chronic fatigue syndrome. Mary A Fletcher, Xiao R Zeng, Zachary Barnes, Silvina Levis and Nancy G Klimas. Journal of Translational Medicine 2009, 7:96
- Cytokine expression profiles of immune imbalance in post-mononucleosis chronic fatigue Gordon Broderick, Ben Z Katz,2 Henrique Fernandes, Mary Ann Fletcher, Nancy Klimas, Frederick A Smith, Maurice RG O’Gorman, Suzanne D Vernon, and Renee Taylo. J Transl Med. 2012; 10 : 191.
- Jason LA, Sorenson M, Porter N, Belkairous N (2010), "An Etiological Model for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome", Neuroscience & Medicine, 2011, 2, 14-27, PMID: 21892413
- Hooper M (2007), "Myalgic encephalomyelitis: a review with emphasis on key findings in biomedical research", J Clin Pathol, May;60(5):466-71, Epub 2006 Aug 25
- Immunology Primer for Practitioners.
IACFS/ME Conference. Translating Science into Clinical Care. March 20-23, 2014 • San Francisco, California, USA
Daniel Peterson, M.D., Griffith University, Gold Coast, Australia, Owner, Sierra Internal Medicine, Incline Village, NV
Sonya Marshall - Gradisnik, BSc (Hons), Ph.D. , Professor of Immunology, Director, National Centre for Neuroimmunology & Emerging Diseases, Griffith University, Australia
Sharni Hardcastle, Ph.D., Research Assistant and Practical Demonstrator , Bond University, Gold Coast, Australia
Nancy Klimas, M.D. Ph.D., Professor of Medicine and Director, NSU COM Institute for Neuro-Immune Medicine Director, Miami VAMC Gulf War Illness and ME/CFS Research Program
Paula Waziry, Ph.D, Assistant Professor, Neuro Immune Medicine, COM, Nova Southeastern University, Miami, Fl
Konstance Knox, Ph.D., Founder, CEO, Coppe Healthcare Solutions
David Baewer, M.D. Ph.D, Medical Director, Coppe Healthcare Solutions
Isabel Barao, Ph.D., Research Assistant Professor, University of Nevada, Reno, Simmaron Research Scientific
Gunnar Gottschalk, B.S., Simmaron Research, Incline Village, NV
Troy Querec, Ph.D., Associate Service Fellow, Centers for Disease Control and Prevention, Atlanta, GA
Dennis Mangan, Ph.D., Chair, Trans-NIH ME/CFS Research Working Group, Office of Research on Women's Health, U.S. National Institutes of Health
Mary Ann Fletcher, Ph.D., University of Miami Miller School of Medicine Professor of Medicine, Microbiology/Immunology and Psychology
Elizabeth Unger, M.D. Ph.D., Chief, Chronic Viral Disease Branch, Division of High-Consequence Pathogens and Pathology, National Center for Emerging and Zoonotic Infectious Diseases. Centers for Disease Control and Prevention, Atlanta, GA
- Plasma cytokines in women with chronic fatigue syndrome. Mary A Fletcher et al. Journal of Translational Medicine 2009, 7:96
- Drexhage R (2011), "Immuno-neuro-endocrine networks. A study on the inflammatory state of circulating monocytes and CD4+ T cells in psychiatric and endocrine autoimmune disease" (proefschrift), Erasmus MC, Rotterdam, ISBN: 978-90-5335-405-6
- Increased nuclear factor-κB and loss of p53 are key mechanisms in Myalgic Encephalomyelitis/chronic fatigue syndrome (ME/CFS). Morris G, Maes M. Med Hypotheses. 2012 Nov;79(5):607-13.
- Cytokine expression as a potential prognostic indicator in post-infectious fatigue. Cytokine. 2010; 52(1–2): SS11–7,81. Link: http://bit.ly/uAfBDS
- In
the book 'Oslers web' the scientific findings showed abnormally high
T-cell helper to T-cell suppressor ratios. Some patients had ratios of over 5:1, and 10:1. Oslers Web, by Hillary Johnson, Penguin Books 1997, page 95
- Oxidative and Nitrosative Stress and Immune-Inflammatory Pathways in Patients with Myalgic Encephalomyelitis (ME)/Chronic Fatigue Syndrome (CFS). Maes et al. Curr Neuropharmacol. 2014 Mar;12(2):168-85.
- Hardcastle SL, Brenu EW, Johnston S, Nguyen T, Huth T, Kaur M, et al. Analysis of
the relationship between immune
dysfunction and symptom severity in patients with
Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (CFS/ME).
J Clin Cell Immunol
(
2014
)
5
:
190.
- Maes M, Twisk FNM, Kubera M, Ringel K: Evidence for inflammation and activation of cell-mediated immunity in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS): increased interleukin-1, tumor necrosis factor-α, PMN-elastase, lysozyme and neopteri. J Affect Disord 2012, 136:933-939.
- TNF-a
and Chronic Fatigue Syndrome. RB. Moss, Journal of Clinical
Immunology, 1999, 19, 5, 314-316
- Host response to infection. Including post-infection phase.
Hickie I, et al. Post-infective and chronic fatigue syndromes precipitated by viral and non-viral pathogens: prospective cohort study. British Journal of Medicine 2006; 333 (7568):575.
- Cytokine expression profiles of immune imbalance in post-mononucleosis chronic fatigue. Gordon Broderick, Ben Z Katz, Henrique Fernandes, Mary Ann Fletcher, Nancy Klimas, Frederick A Smith, Maurice RG O'Gorman, Suzanne D Vernon and Renee Taylor. Journal of Translational Medicine 2012, 10:191.
- Skowera A, Cleare A, Blair D, et al.High levels of type2 cytokine-producing cells in chronic fatigue syndrome.Clin Exp Immunol. 2004;135:294–302.
- Maher KJ, Klimas NG, Fletcher MA: Chronic fatigue syndrome is associated with diminished intracellular perforin. Clin Exp Immunol 2005, 142:505-511.
-
Broderick G, Fuite J, Kreitz A, Vernon SD, Klimas N, Fletcher MA: A formal analysis of cytokine networks in chronic fatigue syndrome. Brain Behav Immun 2010, 24:1209-1217.
-
Maes M, Mihaylova I, Kubera M, Bosmans E: Not in the mind but in the cell: increased production of cyclo-oxygenase-2 and inducible NO synthase in chronic fatigue syndrome. Neuro Endocrinol Lett 2007, 28:463-469.
- Patarca, R. (2001), Cytokines and Chronic Fatigue Syndrome. Annals of the New York Academy of Sciences, 933: 185–200. doi: 10.1111/j.1749-6632.2001.tb05824.x
- Raised levels of proinflammatory cytokines, increased levels of interleukin IL 1 and tumor necrosis factor-α, nuclear factor κB, Increased cyclo-oxygenase 2, IL 2, IL 10, transforming growth factor β, osteopontin levels, neopterin, T regulatory (Treg) dysfunction, Forkhead box P3 (FOXP3) dysfunction, Clonal exhaustion of T cells, raised CD26, CD69 expression, activation of immunoinflammatory pathways.
Gerwyn Morris and Michael Maes. Myalgic encephalomyelitis/chronic fatigue syndrome and encephalomyelitis disseminata/multiple sclerosis show remarkable levels of similarity in phenomenology and neuroimmune characteristics. Morris and Maes BMC Medicine 2013 11:205 doi:10.1186/1741-7015-11-205.
- Buchwald D, Wener MH, Pearlman T, Kith P: Markers of inflammation and immune activation in chronic fatigue and chronic fatigue syndrome. J Rheumatol 1997, 24:372-376.
- I. J. Elenkov, R.L. Wilder, G. P. Chrousos and E. S. Vizi, "The Sympathetic Nerve—An Integrative Interface Between Two Supersystems: The Brain and the Immune System," Pharmacological Reviews, Vol. 52, No. 2, 2000, pp. 595-638.
-
Matsuda J, Gohchi K, Gotch N: Serum concentrations of 2′,5′-oligoadenylate synthetase, neopterin, and beta-glucan in patients with chronic fatigue syndrome and in patients with major depression. J Neurol Neurosurg Psychiatry 1994, 57:1015-1016.
-
Chao CC, Gallagher M, Phair J, Peterson PK: Serum neopterin and interleukin-6 levels in chronic fatigue syndrome. J Infect Dis 1990, 162:1412-1413.
-
Chao CC, Janoff EN, Hu SX, Thomas K, Gallagher M, Tsang M, Peterson PK: Altered cytokine release in peripheral blood mononuclear cell cultures from patients with the chronic fatigue syndrome. Cytokine 1991, 3:292-298
- Kerr JR, Petty R, Burke B, Gough J, Fear D, Sinclair LI, et al. Gene expression
subtypes in patients with chronic fatigue syndrome/myalgic encephalomyelitis.
J Infect
Dis
(
2008
)
197
:
1171
-
1184.
- Lombardi VC, Redelman D, White DC, Fremont M, DeMerirleir K, Peterson D, and Mikovits JA. Serum cytokine and chemokine profiles of individuals with myalgic encephalomyelitis (ME) reveal distinct pathogen associated signatures. September 2008:43(3):245.
- Decreased expression of CD69 in chronic fatigue syndrome in relation to inflammatory markers: evidence for a severe disorder in the early activation of T lymphocytes and natural killer cells.
Mihaylova I, DeRuyter M, Rummens JL, Bosmans E, Maes M.. Neuro Endocrinol Lett. 2007 Aug;28(4):477-83
- Sairenji T, Nagata K. Viral infections in chronic fatigue syndrome] Nippon Rinsho. 2007 Jun;65(6):991-6.
- Lorusso L, Mikhaylova SV, Capelli E, Ferrari D, Ngonga GK, Ricevuti G. Immunological aspects of chronic
fatigue syndrome. Autoimmun Rev. 2009 Feb;8(4):287-91. Epub 2008 Sep 16.
- Serum
levels of some cytokines are often raised in CFS. For example,
levels of interleukin-1 alpha, tumor necrosis factor (TNF) alpha and
TNF-beta were significantly more often increased in CFS patients
-
Hilgers
A, Frank J. Wien Med Wochenschr 1994; 144: 399
-
Linde
A et al. J Infect Dis 1992; 165: 994
-
Patarca
R et al. Clin Infect Dis 1994; 18 suppl 1: S147
-
Hashimoto
N et al. Nippon Rinsho 1992; 50: 2653
-
Bates
DW et al. Arch Intern Med 1995; 155: 97
-
Cytokine
Inflammation and Management in Fibromyalgia and Chronic Fatigue
Syndrome
by John W. Addington
ChronicFatigueSyndromeSupport.com
07-24-2002
-
Immunotherapy
of Chronic Fatigue Syndrome: Therapeutic Interventions Aimed at
Modulating the TH1/TH2 Cytokine Expression Balance
Journal: Journal of Chronic Fatigue Syndrome, Vol.8(1) 2001, pp. 3-37
Authors: Roberto Patarca-Montero, MD, PhD; Nancy G. Klimas, MD; Mary
Ann Fletcher, PhD
-
"A
pilot study of tumour necrosis factor fusion protein, etanercept (a
substance which blocks the interaction of TNF with its cell surface
receptors) was done by K Lambrecht et al (Minneapolis). 6 CFS patients
were given an 8 week trial of etanercept injections. Significant
reductions were observed in the severity of fatigue, muscle pain,
headache and lymphodynia. Exercise tolerance was improved. This lends
support to the theory that proinflammatory cytokines maybe involved in
the pathogenesis of CFS, and this should be further studied in a
placebo-controlled trial. "
K Lambrecht et al (Minneapolis) research paper presented to the AACFS
5th International Research, Clinical and Patient Conference, 2001
-
Roberto
Patarca, Timothy Mark, Mary Ann Fletcher and Nancy Klimas
Review: Immunology of Chronic Fatigue Syndrome
Journal of Chronic Fatigue Syndrome 2000; 6(3/4): 69-107.
-
Popmihajlov Z, Smith KA: Negative feedback regulation of T cells via interleukin-2 and FOXP3 reciprocity. PLoS ONE 2008, 3:e1581.
- Anti-pathogen and immune system treatments. Treatment of 741 italian patients with chronic fatigue syndrome. U. TIRELLI, A. LLESHI, M. BERRETTA, M. SPINA, R. TALAMINI, A. GIACALONE. European Review for Medical and Pharmacological Sciences 2013; 17: 2847-285
- "A
safety and feasibility study of immunomodulation using lymph node
extraction, ex vivo cell culture and autologous cell reinfusion by N
Klimas et al (Miami) found a lack of adverse effects, coupled with
favourable clinical results. 13 patients were studied of which 2 had
unsuitable nodes. The remaining 11 all underwent the procedure
successfully with significant positive clinical outcome over 24 weeks.
An improved cytokine shift correlated with clinical improvement, and
this holds weight to the idea that increases in cytokines lead to
symptoms. At 18 months, improvement is sustained. Further clinical
trials seem warranted. "
N Klimas et al (Miami), research paper presented to the AACFS 5th
International Research, Clinical and Patient Conference, 2001
-
"Downregulation
of Th2 cytokine production with a shift to Th1 cytokine expression was
suggested as a useful intervention in CFS by R Partarco (Miami). Past
approaches have been based on the use of Staphylococcus vaccine,
influenza and/or rubella vaccines and autologous reinfusion of
expanded lymph cells. Further studies are needed to allow elucidation
of factors that mediate Th2-type cytokine expression predominance and
maintenance."
R Partarco (Miami), research paper presented to the AACFS 5th
International Research, Clinical and Patient Conference, 2001
-
"
Cytokines are the chemical messengers of the immune system. Th1 and
Th2 refer to specific cytokine patterns which in the normal immune
system are in balance. Th1 is pro-cytotoxic T cell/ pro antiviral side
and Th2 is the pro-antibody humoral side. Dr. Klimas described that in
healthy individuals, these two systems work like a see-saw - when one
side is up the other is down. In CFS, the Th2 is upregulated with pro
inflammatory TNF-alpha and IL-2. "
SOS (State of the Science) Conference
State of the Science Conference at the National Institutes of Health:
October 23-24, 2000
By Jill McLaughlin, National CFIDS Foundation, USA
- "Dr.
Gupta did in vitro study and found unstimulated CFS cells, which
should be doing nothing, were producing TNF-alpha. Klimas had shown
mRNA for TNF alpha up regulated as well as the actual peptide in
circulation which she states is "truly remarkable" because
cytokines are a lymph node phenomenon and are not supposed to be in
peripheral blood but in 29% of patients in their study they measured
actual TNF peptide.
More important than cross sectional studies of cytokines is the need
to do more studies of cytokine expression over time and what it might
be related to. Klimas has done studies of patterns of cytokine
expression over time and noted that they change with illness severity
with pro-inflammatory Th2 pattern increasing during times of flare.
Also a cluster analysis in literature show TNF cluster with IL1 and
TH2 type cytokines being expressed."
SOS (State of the Science) Conference
State of the Science Conference at the National Institutes of Health:
October 23-24, 2000
By Jill McLaughlin, National CFIDS Foundation, USA
-
Reserach
presented by Dr. William Carter to the 31st Interscience Conference on
Antimicrobial Agents and Chemotherapy
Dr. Carter told the Conference Journal that his research group had
determined that more than two-thirds of CFS patients have abnormally
high levels of lymphokines; because of that, he suggested that CFS
might more appropriately be named "lymphokine overdose
disease." According to Dr. Carter, many of the symptoms of CFS --
such as fatigue, memory loss, and other problems with thinking -- are
probably caused by the high levels of lymphokines that patients are
making in their own bodies.
Dr. William A. Carter is a Professor of Oncology and Hematology at
Hahnemann University in Philadelphia
-
Abnormally
high levels of IL-2 have consistently been found in CFS patients by
researchers. The IL-2 levels exceeded those found in MS patients, AIDS
patients and Lymphoma patients.
Oslers Web, by Hillary Johnson, Penguin Books 1997, pages 321-322
-
Cheney PR, Dorman SE, Bell DS: Interleukin-2 and the chronic fatigue syndrome. Ann Intern Med 1989, 110:321.
-
"A
poster presentation by P Clifton Bligh et al (NSW) concluded that the
fall in urinary succinic acid seen in CFS patients was associated with
deregulation of energy availability and protein synthesis suggestive
of a cytokine mediated nitric oxide mediated change in chemistry.
These changes relate to the expression of fatigue."
Research paper presented by P Clifton Bligh et al (NSW) to The Sydney
ME / CFS Clinical and Scientific Conference, December 2001
-
Klimas,
Cytokine and Other Immunologic Markers in Chronic Fatigue Syndrome and
Their Relation to Neuropsychological Factors, Applied Neuropsychology,
8(1);51 (2001)
- Klimas N, Koneru AO: Chronic fatigue syndrome: inflammation, immune function, and neuroendocrine interactions. Curr Rheumatol Rep 2007, 9:482-487.
-
Capelli E, Zola R, Lorusso L, Venturini L, Sardi F, Ricevuti G: Chronic fatigue syndrome/myalgic encephalomyelitis: an update. Int J Immunopathol Pharmacol 2010, 23:981-989.
-
Klimas,
Nancy G., Fernando R. Salvato, Robert Morgan, and Mary Ann Fletcher;
"Immunologic Abnormalities in Chronic Fatigue Syndrome";
Journal of Clinical Microbiology 28(6):1403, June 1990.
-
Mullington,
et al., Mediators of Inflammation and Their Interaction with Sleep:
Relevance for Chronic Fatigue Syndrome and Related Conditions, Annals
of the New York Academy of Sciences, 933:201 (2001)
- Wallace,
et al., Cytokines Play an Aetiopathogenetic Role in Fibromyalgia: a
Hypothesis and Pilot Study, Rheumatology, 40:743 (2001)
-
Rheumatology.HSS.edu,
Cytokines in Inflammatory Disease (Interview of Lionel Ivashkiv)
(2002) http://www.rheumatology.hss.edu/phys/interviews/ivashkiv_int_tran.asp
-
AFSA,
Cytokine Abnormalities Official, AFSA Update, 8(2) (2002)
-
Patarca,
Cytokines and Chronic Fatigue Syndrome, Annals of the New York Academy
of Sciences, 933:185 (2001)
(e) B cell Abnormalities, Autoimmunity factors
- Kappa/Lambda assay test
In the book Osler's Web: Inside the Labyrinth of the Chronic Fatigue Syndrome Epidemic by Hillary Johnson where medical doctors in the USA found an unusually high number of B cell lymphomas in ME patients. Special scientific tests showed that these B-cell Lymphomas in ME patients were unusual types, not seen before. The researchers also found B-cell deficiency in all patients, and a positive result on the kappa/lambda assay for a majority of these patients. After studying samples from approximately fifty patients, Wormsley estimated that the rate of clonal excess abnormality in the CFS patients from Nevada was at least 25 percent ('Oslers Web, by Hillary Johnson, Penguin Books 1997, page 94). This is significant as kappa/lambda light chains are the result of abnormalities within the bone marrow B-cell lineage. This has direct on B-cells and overall immunity, and susceptibility to Cancers. Recent scientific studies show that the incidence rate of non-Hodgkin's lymphoma is 0.02% in the United States, yet nearly 5% of CFS patients develop the disease. This is a significant risk factor. by Hillary Johnson where medical doctors in the USA found an unusually high number of B cell lymphomas in ME patients. Special scientific tests showed that these B-cell Lymphomas in ME patients were unusual types, not seen before. The researchers also found B-cell deficiency in all patients, and a positive result on the kappa/lambda assay for a majority of these patients. After studying samples from approximately fifty patients, Wormsley estimated that the rate of clonal excess abnormality in the CFS patients from Nevada was at least 25 percent ('Oslers Web, by Hillary Johnson, Penguin Books 1997, page 94). This is significant as kappa/lambda light chains are the result of abnormalities within the bone marrow B-cell lineage. This has direct on B-cells and overall immunity, and susceptibility to Cancers. Recent scientific studies show that the incidence rate of non-Hodgkin's lymphoma is 0.02% in the United States, yet nearly 5% of CFS patients develop the disease. This is a significant risk factor.
- Gamma T cell clonal rearrangement
This tests for pre-Cancerous conditions related to ME . A certain percentage of ME patients are at high risk of getting B cell Lymphoma and other Cancers. This test is recommended by Dr. Dan Peterson who has been involved in treating ME pateints and in sceintific research since the early 1990's.
- B-Cell Phenotyping Profile for Immunodeficiency and Immune Competence Assessment, Blood
http://www.mayomedicallaboratories.com/test-catalog/Clinical+and+Interpretive/88800
- B call activation. Elevated B-cells with CD20 marker (ME Primer for Healthcare Professionals: based on Myalgic encephalomyelitis: International Consensus Criteria, 2012)
- Naïve B cells are a high percentage of all B cells. Lowered levels of IL 21,12, and 27, which h are involved in the maturation of B cells. These immature B-cells cannot properly target infections. Invest in ME Scientific Conference 2013 (Dr. Amolok Bansal).
- Bansal et al. found the following in ME patients in 2012 and 2013
' patients had greater numbers of naive B cells as a percentage of lymphocytes: 6·3 versus 3·9% in HC (P = 0·034), greater numbers of naive B cells as a percentage of B cells: 65 versus 47% in controls (P = 0·003), greater numbers of transitional B cells: 1·8 versus 0·8% in controls (P = 0·025) and reduced numbers of plasmablasts: 0·5 versus 0·9% in controls (P = 0·013). While the cause of these changes is unclear, we speculate whether they may suggest a subtle tendency to autoimmunity.'
Bansal et al., (2013), Altered functional B cell subset populations in patients with chronic fatigue syndrome compared to healthy controls. Clinical & Experimental Immunology, 172: 73–80.
- B cells with CD20 marker
(Important regarding drug Rituximab which was used many years later)
- Klimas, N. G., F. R. Salvato, R. Morgan, and M. A. Fletcher. 1990. Immunologic abnormalities in chronic fatigue syndrome. J. Clin. Microbiol. 28:1403-1410.
- Tirelli, U., A. Pinto, G. Marotta, M. Crovato, M. Quaia, P. De Paoli, E. Galligioni, and G. Santini. 1993. Clinical and immunologic study of 205 patients with chronic fatigue syndrome: a case series from Italy. Arch. Intern. Med. 153:116-117.
- Rituximab trials for ME/CFS
Rituximab reduces or eliminates CD20+ B cells, reduces Th17 T cell production, reduces Il 2 levels and the production of NFκB.
- Clinical impact of B-cell depletion with the anti-CD20 antibody rituximab in chronic fatigue syndrome: a preliminary case series
- Benefit from B-Lymphocyte Depletion Using the Anti-CD20 Antibody Rituximab in Chronic Fatigue Syndrome. A Double-Blind and Placebo-Controlled Study
- B-Lymphocyte Depletion in Myalgic Encephalopathy/ Chronic Fatigue Syndrome. An Open-Label Phase II Study with Rituximab Maintenance Treatment.Øystein Fluge ,
Kristin Risa,
Sigrid Lunde,
Kine Alme,
Ingrid Gurvin Rekeland,
Dipak Sapkota,
Einar Kleboe Kristoffersen,
Kari Sørland,
Ove Bruland,
Olav Dahl,
Olav Mella
- Antibodies to β adrenergic and muscarinic cholinergic receptors in patients with Chronic Fatigue Syndrome. Madlen Loebela, Patricia Grabowskia, Harald Heideckeb, Sandra Bauera, Leif G. Hanitscha, Kirsten Wittkea, Christian Meisela, c, Petra Reinked, e, Hans-Dieter Volka, e, Øystein Flugef, Olav Mellaf, g, Carmen Scheibenbogena, e. Brain, Behavior, and Immunity
Volume 52, February 2016, Pages 32–39.
Rituximab use and trials in Multiple Scelorisis and Rheumatoid Arthritis and other autoimmune illnesses
-
Hauser SL, Waubant E, Arnold DL, Vollmer T, Antel J, Fox RJ, Bar-Or A, Panzara M, Sarkar N, Agarwal S, Langer-Gould A, Smith CH, HERMES Trial Group: B-cell depletion with rituximab in relapsing-remitting multiple sclerosis. New Engl J Med 2008, 358:676-68
-
Monson NL, Cravens PD, Frohman EM, Hawker K, Racke MK: Effect of rituximab on the peripheral blood and cerebrospinal fluid B cells in patients with primary progressive multiple sclerosis. Arch Neurol 2005, 62:258-264
-
Cross AH, Stark JL, Lauber J, Ramsbottom MJ, Lyons JA: Rituximab reduces B cells and T cells in cerebrospinal fluid of multiple sclerosis patients. J Neuroimmunol 2006, 180:63-70
-
Bar-Or A, Fawaz L, Fan B, Darlington PJ, Rieger A, Ghorayeb C, Calabresi PA, Waubant E, Hauser SL, Zhang J, Smith CH: Abnormal B-cell cytokine responses a trigger of T-cell-mediated disease in MS? Ann Neurol 2010, 67:452-461
-
Reichardt P, Dornbach B, Rong S, Beissert S, Gueler F, Loser K, Gunzer M: Naive B cells generate regulatory T cells in the presence of a mature immunologic synapse. Blood 2007, 110:1519-1529.
-
Emery P, Fleischmann R, Filipowicz-Sosnowska A, Schechtman J, Szczepanski L, Kavanaugh A, Racewicz AJ, van Vollenhoven RF, Li NF, Agarwal S, Hessey EW, Shaw TM, DANCER Study Group: The efficacy and safety of rituximab in patients with active rheumatoid arthritis despite methotrexate treatment: results of a phase IIB randomized, double-blind, placebo-controlled, dose-ranging trial. Arthritis Rheum 2006, 54:1390-1400
-
Eisenberg R: Update on rituximab. Ann Rheum Dis 2005, 64:iv55-iv57.
-
Gurcan HM, Keskin DB, Stern JN, Nitzberg MA, Shekhani H, Ahmed AR: A review of the current use of rituximab in autoimmune diseases. Int Immunopharmacol 2009, 9:10-25
-
Edwards JC, Szczepanski L, Szechinski J, Filipowicz-Sosnowska A, Emery P, Close DR, Stevens RM, Shaw T: Efficacy of B-cell-targeted therapy with rituximab in patients with rheumatoid arthritis. N Engl J Med 2004, 350:2572-2581. 
-
Cohen SB, Emery P, Greenwald MW, Dougados M, Furie RA, Genovese MC, Keystone EC, Loveless JE, Burmester GR, Cravets MW, Hessey EW, Shaw T, Totoritis MC, REFLEX Trial Group: Rituximab for rheumatoid arthritis refractory to anti-tumor necrosis factor therapy: results of a multicenter, randomized, double-blind, placebo-controlled, phase III trial evaluating primary efficacy and safety at twenty-four weeks. Arthritis Rheum 2006, 54:2793-2806. 
-
Tokunaga M, Saito K, Kawabata D, Imura Y, Fujii T, Nakayamada S, Tsujimura S, Nawata M, Iwata S, Azuma T, Mimori T, Tanaka Y: Efficacy of rituximab (anti-CD20) for refractory systemic lupus erythematosus involving the central nervous system. Ann Rheum Dis 2007, 66:470-475. 
-
Devauchelle-Pensec V, Pennec Y, Morvan J, Pers JO, Daridon C, Jousse-Joulin S, Roudaut A, Jamin C, Renaudineau Y, Roue IQ, Cochener B, Youinou P, Saraux A: Improvement of Sjogren’s syndrome after two infusions of rituximab (anti-CD20). Arthritis Rheum 2007, 57:310317.
- van de Veerdonk FL, Lauwerys B, Marijnissen RJ, Timmermans K, Di Padova F, Koenders MI, Gutierrez-Roelens I, Durez P, Netea MG, van der Meer JW, van den Berg WB, Joosten LA: The anti-CD20 antibody rituximab reduces the Th17 cell response. Arthritis Rheum 2011, 63:1507-1
- Magnusson M, Brisslert M, Zendjanchi K, Lindh M, Bokarewa MI (2010), "Epstein-Barr virus in bone marrow of rheumatoid arthritis patients predicts response to rituximab treatment", Rheumatology (Oxford), Oct;49(10):1911-9, Epub 2010 Jun 14
- "Loebel M, Strohschein K, Giannini C, Koelsch U, Bauer S, Doebis C, Thomas S, Unterwalder N, Von Baehr V, Reinke P, Knops M, Hanitsch LG, Meisel C, Volk H-D, Scheibenbogen C (2014), "Deficient EBV-Specific B- and T-Cell Response in Patients with Chronic Fatigue Syndrome", PLoS ONE 9(1): e85387.
- Antibodies to β adrenergic and muscarinic cholinergic receptors in patients with Chronic Fatigue Syndrome. Madlen Loebela, Patricia Grabowskia, Harald Heideckeb, Sandra Bauera, Leif G. Hanitscha, Kirsten Wittkea, Christian Meisela, c, Petra Reinked, e, Hans-Dieter Volka, e, Øystein Flugef, Olav Mellaf, g, Carmen Scheibenbogena, e. Brain, Behavior, and Immunity
Volume 52, February 2016, Pages 32–39.
- Immunology Primer for Practitioners.
IACFS/ME Conference. Translating Science into Clinical Care. March 20-23, 2014 • San Francisco, California, USA
Daniel Peterson, M.D., Griffith University, Gold Coast, Australia, Owner, Sierra Internal Medicine, Incline Village, NV
Sonya Marshall - Gradisnik, BSc (Hons), Ph.D. , Professor of Immunology, Director, National Centre for Neuroimmunology & Emerging Diseases, Griffith University, Australia
Sharni Hardcastle, Ph.D., Research Assistant and Practical Demonstrator , Bond University, Gold Coast, Australia
Nancy Klimas, M.D. Ph.D., Professor of Medicine and Director, NSU COM Institute for Neuro-Immune Medicine Director, Miami VAMC Gulf War Illness and ME/CFS Research Program
Paula Waziry, Ph.D, Assistant Professor, Neuro Immune Medicine, COM, Nova Southeastern University, Miami, Fl
Konstance Knox, Ph.D., Founder, CEO, Coppe Healthcare Solutions
David Baewer, M.D. Ph.D, Medical Director, Coppe Healthcare Solutions
Isabel Barao, Ph.D., Research Assistant Professor, University of Nevada, Reno, Simmaron Research Scientific
Gunnar Gottschalk, B.S., Simmaron Research, Incline Village, NV
Troy Querec, Ph.D., Associate Service Fellow, Centers for Disease Control and Prevention, Atlanta, GA
Dennis Mangan, Ph.D., Chair, Trans-NIH ME/CFS Research Working Group, Office of Research on Women's Health, U.S. National Institutes of Health
Mary Ann Fletcher, Ph.D., University of Miami Miller School of Medicine Professor of Medicine, Microbiology/Immunology and Psychology
Elizabeth Unger, M.D. Ph.D., Chief, Chronic Viral Disease Branch, Division of High-Consequence Pathogens and Pathology, National Center for Emerging and Zoonotic Infectious Diseases. Centers for Disease Control and Prevention, Atlanta, GA
- "Kenny
de Meirleir and his group looked at the association between
mycoplasmae and the 2-5A/RNaseL pathway in CFS. The hypothesis was
that there maybe a co-morbid physiopathological mechanism between
Mycoplasma infection and the deregulation of the pathway. 182 mainly
female patients, free of antibiotic treatment were enrolled. There was
significant correlation. He showed that mycoplasmae are active in
stimulating some components of the immune system. They can act as
polyclonal T cell and B cell activators. Monocytes produce elastase,
which can cleave 80kDa RNaseL thus causing deregulation of the
antiviral pathway. It has been suggested that LMW RNaseL may reduce
Th1 activity, which implicates susceptibility to infections and a
suppressed ability to eliminate intracellular antigens."
Research paper presented by Kenny de Meirleir (Brussels, Belgium) to
The Sydney ME / CFS Clinical and Scientific Conference, December 2001
-
The following diagram by Knox et al. (2011) shows some of the autoimmunity factors found in ME.
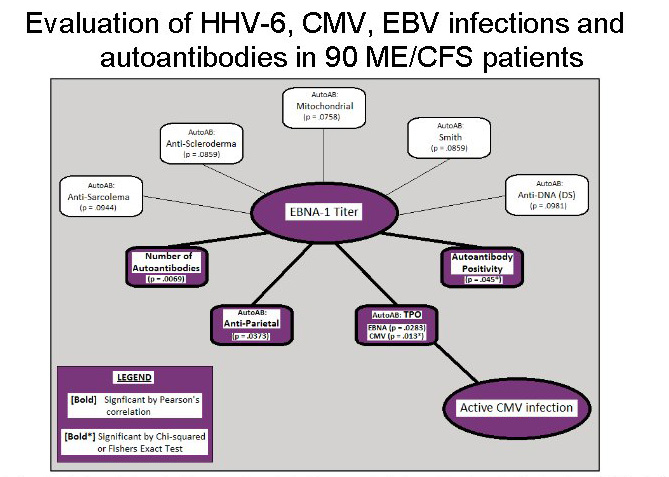
Source: Knox, K., et al. Systemic Leukotropic Herpesvirus Infections and Autoantibodies in Patients with Myalgic Encephalomyelitis – Chronic Fatigue Syndrome. 7th International Conference on HHV-6 and 7. March 1, 2011. Reston, VA..
- Clinical Activity of Folinic Acid in Patients with Chronic Fatigue Syndrome
- In the book Osler's Web: Inside the Labyrinth of the Chronic Fatigue Syndrome Epidemic
 by Hillary Johnson where medical doctors in the USA found an unusually high number of B cell lymphomas in ME patients. Special scientific tests showed that these B-cell Lymphomas in ME patients were unusual types, not seen before. The researchers also found B-cell deficiency in all patients, and a positive result on the kappa/lambda assay for a majority of these patients. After studying samples from approximately fifty patients, Wormsley estimated that the rate of clonal excess abnormality in the CFS patients from Nevada was at least 25 percent ('Oslers Web, by Hillary Johnson, Penguin Books 1997, page 94). This is significant as kappa/lambda light chains are the result of abnormalities within the bone marrow B-cell lineage. This has direct on B-cells and overall immunity, and susceptibility to Cancers. Recent scientific studies show that the incidence rate of non-Hodgkin's lymphoma is 0.02% in the United States, yet nearly 5% of CFS patients develop the disease. This is a significant risk factor. by Hillary Johnson where medical doctors in the USA found an unusually high number of B cell lymphomas in ME patients. Special scientific tests showed that these B-cell Lymphomas in ME patients were unusual types, not seen before. The researchers also found B-cell deficiency in all patients, and a positive result on the kappa/lambda assay for a majority of these patients. After studying samples from approximately fifty patients, Wormsley estimated that the rate of clonal excess abnormality in the CFS patients from Nevada was at least 25 percent ('Oslers Web, by Hillary Johnson, Penguin Books 1997, page 94). This is significant as kappa/lambda light chains are the result of abnormalities within the bone marrow B-cell lineage. This has direct on B-cells and overall immunity, and susceptibility to Cancers. Recent scientific studies show that the incidence rate of non-Hodgkin's lymphoma is 0.02% in the United States, yet nearly 5% of CFS patients develop the disease. This is a significant risk factor.
- Tirelli U, Marotta G, Improta S, Pinto A: Immunological abnormalities in patients with chronic fatigue syndrome. Scand J Immunol 40(6):601-608, 1994
- The Dubbo Studies which were published in leading medical journals point to genetic factors, environmental factors and a post-infectious dysfunctional immune system as being the key factors in ME / CFS.
Post-infective and chronic fatigue syndromes precipitated by viral and non-viral pathogens: prospective cohort study. Hickie I, Davenport T, Wakefield D, Vollmer-Conna U, Cameron B, Vernon SD, Reeves WC, Lloyd A; Dubbo Infection Outcomes Study Group.
BMJ. 2006 Sep 16;333(7568):575. Epub 2006 Sep 1.
Cytokine polymorphisms have a synergistic effect on severity of the acute sickness response to infection.
Vollmer-Conna U, Piraino BF, Cameron B, Davenport T, Hickie I, Wakefield D, Lloyd AR; Dubbo Infection Outcomes Study Group.
Clin Infect Dis. 2008 Dec 1;47(11):1418-25. doi: 10.1086/592967.
- Staines DR
. Do vasoactive neuropeptides and heat shock proteins mediate fatigue-
related autoimmune disorders?
Med Hypotheses.
2005;64(3):539-42. PMID: 15617862
- Klimas N, Salvato F, Morgan R, Fletcher MA: Immunologic abnormalities in chronic fatigue syndrome. J Clin Microbiol 28(6):1403-1410, 1990
- "B
cell function in vitro shows reduced responses to viral antigens but
enhanced responses to allergens with goes along with cytokine
dysfunction. In vivo, twelve of eighteen studies have show
abnormalities in immunoglobulin expression. IgG1 and IgG3 subclasses
are the two most responsible in containing viruses. Six studies have
shown abnormally low levels of IgG1 and IgG3.
Of twelve studies of NK cell function in CFS, ten have showed low NK
cell function. More interesting is NK response to cytokine
manipulation in vitro -several studies suggest NK cells in CFS do not
respond normally to IL-2 or gamma interferon and that gamma interferon
may be impaired. This raises the question of cellular exhaustion in
system that is constantly activated - how long can it be "turned
on" and be able to be responsive? Dr. Suhadolnik's studies in the
literature look at elevation of an anti-viral induction pathway and
found abnormal production of a critical enzyme."
SOS (State of the Science) Conference
State of the Science Conference at the National Institutes of Health:
October 23-24, 2000
By Jill McLaughlin, National CFIDS Foundation, USA
- Autoimmune disease: A role for new anti-viral therapies? Dreyfus DH. Autoimmun Rev. 2011 Dec;11(2):88-97
- Hardcastle SL, Brenu EW, Johnston S, Nguyen T, Huth T, Kaur M, et al. Analysis of
the relationship between immune
dysfunction and symptom severity in patients with
Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (CFS/ME).
J Clin Cell Immunol
(
2014
)
5
:
190.
- Antilamin antibodies
There is evidence of Antilamin antibodies in many ME patients (Findings of Dr. Malcolm Hooper. Anti-nuclear envelope antibodies: Clinical associations. Semin Arthritis Rheum 2001 Apr;30(5):313-320 Nesher G, Margalit R, Ashkenazi YJ.). This test can be carried out in a major hospital.
- Autoantibodies to insoluble cellular antigens (vimentin and lamin B1)
von Mikecz A, Konstantinov K, Buchwald DS, Gerace L, Tan EM: High frequency of autoantibodies in patients with chronic fatigue syndrome. Arthritis & Rheumatism 40(2):295-305, 1997
- Knox, K., et al. Systemic Leukotropic Herpesvirus Infections and Autoantibodies in Patients with Myalgic Encephalomyelitis – Chronic Fatigue Syndrome. 7th International Conference on HHV-6 and 7. March 1, 2011. Reston, VA.
- Autoantibodies to Nuclear Envelope Antigens
Autoantibodies to Nuclear Envelope Antigens in Chronic Fatigue Syndrome. K Konsintinov, Dedra Buchwald, J Jones et al J Clin Invest 1996:98:8:1888-1896
- Anti-neuronal antibody level
Buchwald MD, Wener MH, Komaroff AL: Antineuronal antibody levels in chronic fatigue syndrome patients with neurologic abnormalities. Arthritis Rheum 1991, 34:1485-1486.
- Abnormal levels of HLA-DQ3 (Keller et al, 1992)
- "Autoimmune responses directed against disrupted lipid membrane components (palmitic, myristic and oleic acid), and residue molecules of lipid peroxidation, such as azelaic acid and malondialdehyde, IgM responses against the S-farnesyl-L-cysteine, and amino acids, modified by nitrating species such as nitrotyrosine, nitrophenylalanine, nitrotryptophan, nitroarginine and nitrocysteine, have all been reported"
Myalgic encephalomyelitis/chronic fatigue syndrome and encephalomyelitis disseminata/multiple sclerosis show remarkable levels of similarity in phenomenology and neuroimmune characteristics. Gerwyn Morris, Michael Maes. BMC Medicine 2013, 11:205 doi:10.1186/1741-7015-11-205
- Nishikai M: Antinuclear antibodies in patients with chronic fatigue syndrome. Nippon Rinsho 2007, 65:1067-1070.
- Oxidative and Nitrosative Stress and Immune-Inflammatory Pathways in Patients with Myalgic Encephalomyelitis (ME)/Chronic Fatigue Syndrome (CFS). Maes et al. Curr Neuropharmacol. 2014 Mar;12(2):168-85.
-
Bassi N, Amital D, Amital H, Doria A, Shoenfeld Y: Chronic fatigue syndrome: characteristics̃and possible causes for its pathogenesis. Isr Med Assoc J 2008, 10:79-82.
-
Klein R, Berg PA: High incidence of antibodies to 5-hydroxytryptamine, gangliosides and phospholipids in patients with chronic fatigue and fibromyalgia syndrome and their relatives: evidence for a clinical entity of both disorders. Eur J Med Res 1995, 1:21-26.
- Nijs J, McGregor NR, De Becker P, Verhas M, Englebienne P, De Meirleir K: Monitoring a hypothetical channelopathy in chronic fatigue syndrome: preliminary observations. JCFS 2003, 11:117-133.
-
Nijs J, Coomans D, Nicolson GL, De Becker P, Christian D, De Meirleir K: Immunophenotyping predictive of mycoplasma infection in patients with chronic fatigue syndrome. JCFS 2003, 11:51-69
-
Tanaka S, Kuratsune H, Hidaka Y, Hakariya Y, Tatsumi KI, Takano T, Kanakura Y, Amino N: Autoantibodies against muscarinic cholinergic receptor in chronic fatigue syndrome. Int J Mol Med 2003, 12:225-230.
- Maes M, Mihaylova I, Leunis JC: Chronic fatigue syndrome is accompanied by an IgM-related immune response directed against neopitopes formed by oxidative or nitrosative damage to lipids and proteins. Neuro Endocrinol Lett 2006, 27:615-621
-
Tirelli U, Marotta G, Improta S, Pinto A: Immunological abnormalities in patients with chronic fatigue syndrome. Scand J Immunol 1994, 40:601-608.
- Kerr JR, Petty R, Burke B, Gough J, Fear D, Sinclair LI, et al. Gene expression
subtypes in patients with chronic fatigue syndrome/myalgic encephalomyelitis.
J Infect
Dis
(
2008
)
197
:
1171
-
1184.
- Anderton SM, Fillatreau S: Activated B cells in autoimmune diseases: the case for a regulatory role. Nat Clin Pract Rheumatol 2008, 4:657-666
- Antinuclear Envelope Antibodies Clinical Associations. Nesher G, Margalit R, Ashkenazi YJ Semin Arthritis Rheum 2001:30: (5):313-320
- Anticardiolipin Antibodies in the Sera of Patients with Diagnosed Chronic Fatigue Syndrome Yoshitsugi Hokama, Cara Empey Campora, Cynthia Hara, Tina Kuribayashi, Diana Le Huynh, and Kenichi Yabusaki. Department of Pathology, John A. Burns School of Medicine, University of Hawaii at Maˆnoa, Honolulu, Hawaii. Journal of Clinical Laboratory Analysis 23 : 210–212 (2009)
- Hokama Y, Empey-Campora C, Hara C, et al. Acute phase phospholipids related to the cardiolipin of mitochondria in the sera of patients with chronic fatigue syndrome (CFS) chronic ciguatera fish poisoning (CCFP), and other diseases attributed to chemicals, Gulf War, and marine toxins. J Clin Lab Anal 2008;22:99–105.
- Boullerne A, Petry KG, Geffard M: Circulating antibodies directed against conjugated fatty acids in sera of patients with multiple sclerosis. J Neuroimmunol 1996, 65:75-81
- Knox, K., et al. Systemic Leukotropic Herpesvirus Infections and Autoantibodies in Patients with Myalgic Encephalomyelitis – Chronic Fatigue Syndrome. 7th International Conference on HHV-6 and 7. March 1, 2011. Reston, VA.
- Important scientific findings in the book Osler's Web: Inside the Labyrinth of the Chronic Fatigue Syndrome Epidemic
 by Hillary Johnson where medical doctors in the USA found an unusually high number of B cell lymphomas in ME / CFS patients. Special scientific tests showed that these B-cell Lymphomas in ME / CFS patients were unusual types, not seen before. The researchers also found B-cell deficiency in all patients, and a positive result on the kappa/lambda assay for a majority of these patients. This is significant as kappa/lambda light chains are the result of abnormalities within the bone marrow B-cell lineage. This has direct on B-cells and overall immunity, and susceptibility to Cancers. Recent scientific studies show that the incidence rate of non-Hodgkin's lymphoma is 0.02% in the United States, yet nearly 5% of CFS patients develop the disease. This is a significant risk factor by Hillary Johnson where medical doctors in the USA found an unusually high number of B cell lymphomas in ME / CFS patients. Special scientific tests showed that these B-cell Lymphomas in ME / CFS patients were unusual types, not seen before. The researchers also found B-cell deficiency in all patients, and a positive result on the kappa/lambda assay for a majority of these patients. This is significant as kappa/lambda light chains are the result of abnormalities within the bone marrow B-cell lineage. This has direct on B-cells and overall immunity, and susceptibility to Cancers. Recent scientific studies show that the incidence rate of non-Hodgkin's lymphoma is 0.02% in the United States, yet nearly 5% of CFS patients develop the disease. This is a significant risk factor
- Dr. Uckun et al , recently published a paper 'Clinical Activity of Folinic Acid in Patients with Chronic Fatigue Syndrome' In this article, the researchers found that 94% of the CFS patients had a B-cell immunodeficiency with a marked depletion of their CD19+IgM+ mature B-lymphocyte population. The CD19+IgM+ cells ranged from a low of 0.5% to a high of 53%. These researchers concluded that there was "a high incidence of severe B-cell immunodeficiency" in CFS patients. This correlates to clinical and scientific findings in the book Osler's Web mentioned above.
- HHV-6a virus which has been consistently found in high pecentages of ME / CFS patients has been found to be
associated with Hodgkin's lymphoma, acute lymphocytic leukemia,
African Burkitts lymphoma, and sarcoidosis, as well as
AIDS and Chronic Fatigue Syndrome. Lusso, P. et al.;
"In Vitro Cellular Tropism of Human B-Lymphotropic Virus(Human
Herpesvirus-6)"; Journal of Experimental Medicine 167:1659, May
1988.
(f)
Cleavage of all six insulin-like growth
factor binding proteins (IGFBPs) with a significant proteolytic cleavage
of IGFBP-3
(g) Neuropeptide Dysfunction
- Staines DR. Is chronic fatigue syndrome an autoimmune disorder of endogenous neuropeptides, exogenous infection and molecular mimicry? Med Hypotheses2004;62(5):646-52.
- Plasma neuropeptide Y: a biomarker for symptom severity in chronic fatigue syndrome. Fletcher, MA, Rosenthal M, Antoni M, Ironson G, Zeng XR, Barnes Z, Harvey JM, Hurwitz B, Levis S, Broderick G and Klimas NG. Behavioral and Brain Functions 2010, 6:76
- Vigna-Perez M, Hernandez-Castro B, Paredes-Saharopulos O, Portales-Perez D, Baranda L, Abud-Mendoza C, Gonzalez-Amaro R: Clinical and immunological effects of rituximab in patients with lupus nephritis refractory to conventional therapy: a pilot study. Arthritis Res Ther 2006, 8:R83.
-
Vigna-Perez M, Abud-Mendoza C, Cuevas-Orta E, Baranda L, Paredes-Saharopulos O, Moreno R, Gonzalez-Amaro R: In vivo effect of rituximab on regulatory T cells and apoptosis in patients with rheumatoid arthritis. Immunologia 2006, 25:167-172.
- Staines DR
. Do vasoactive neuropeptides and heat shock proteins mediate fatigue-
related autoimmune disorders?
Med Hypotheses.
2005;64(3):539-42. PMID: 15617862
- Host response to infection. Including post-infection phase.
Hickie I, et al. Post-infective and chronic fatigue syndromes precipitated by viral and non-viral pathogens: prospective cohort study. British Journal of Medicine 2006; 333 (7568):575.
- Immunology Primer for Practitioners.
IACFS/ME Conference. Translating Science into Clinical Care. March 20-23, 2014 • San Francisco, California, USA
Daniel Peterson, M.D., Griffith University, Gold Coast, Australia, Owner, Sierra Internal Medicine, Incline Village, NV
Sonya Marshall - Gradisnik, BSc (Hons), Ph.D. , Professor of Immunology, Director, National Centre for Neuroimmunology & Emerging Diseases, Griffith University, Australia
Sharni Hardcastle, Ph.D., Research Assistant and Practical Demonstrator , Bond University, Gold Coast, Australia
Nancy Klimas, M.D. Ph.D., Professor of Medicine and Director, NSU COM Institute for Neuro-Immune Medicine Director, Miami VAMC Gulf War Illness and ME/CFS Research Program
Paula Waziry, Ph.D, Assistant Professor, Neuro Immune Medicine, COM, Nova Southeastern University, Miami, Fl
Konstance Knox, Ph.D., Founder, CEO, Coppe Healthcare Solutions
David Baewer, M.D. Ph.D, Medical Director, Coppe Healthcare Solutions
Isabel Barao, Ph.D., Research Assistant Professor, University of Nevada, Reno, Simmaron Research Scientific
Gunnar Gottschalk, B.S., Simmaron Research, Incline Village, NV
Troy Querec, Ph.D., Associate Service Fellow, Centers for Disease Control and Prevention, Atlanta, GA
Dennis Mangan, Ph.D., Chair, Trans-NIH ME/CFS Research Working Group, Office of Research on Women's Health, U.S. National Institutes of Health
Mary Ann Fletcher, Ph.D., University of Miami Miller School of Medicine Professor of Medicine, Microbiology/Immunology and Psychology
Elizabeth Unger, M.D. Ph.D., Chief, Chronic Viral Disease Branch, Division of High-Consequence Pathogens and Pathology, National Center for Emerging and Zoonotic Infectious Diseases. Centers for Disease Control and Prevention, Atlanta, GA
(h) HLA abnormalities. Often associated with abnormal CD38 levels.
It is worth noting that relatively high proportions of HLA-DR+ T cells have been reported in a number of autoimmune disorders.
- 4 to 6 fold increased relative risk for DR4, DR3
and DQ3 (Keller et al, 1992)
- HLA DR haplotypes in 112 South Florida CFS
patients, compared to 5,000 regional and
national controls. (Klimas et al., 2007)
- HLA-DR4 positive. Chronic Fatigue Syndrome. JA Goldstein. pub: The Chronic Fatigue Syndrome Institute, Beverly Hills, California 1990 ISBN 0-9625654-0-7
- Lloyd, A. R., D. Wakefield, C. R. Boughton, and J. M. Dwyer. 1989. Immunological abnormalities in the chronic fatigue syndrome. Med. J. Austral. 151:122-124.
- HLA-DQA1. Association of chronic fatigue syndrome with human leucocyte antigen class II alleles. J Smith, E L Fritz, J R Kerr, A J Cleare, S Wessely, and D L Mattey. J Clin Pathol. 2005 August; 58(8): 860–863.
- HLA DR abnormalities. Chronic fatigue syndrome: clinical condition associated with immune activation. A.L. Landay, E.T. Lennette, C. Jessop, J.A. Levy. The Lancet, Volume 338, Issue 8769, 21 September 1991, Pages 707-712.
- Immunologic Abnormalities Associated with Chronic Fatigue Syndrome Edward Barker, Sue F. Fujimura, Mitchell B. Fadem, Alan L. Landay, andJay A. Levy
- Klimas N, Salvato F, Morgan R, Fletcher MA: Immunologic abnormalities in chronic fatigue syndrome. J Clin Microbiol 28(6):1403-1410, 1990
- Hassan IS, Bannister BA, Akbar A, Weir W, Bofill M: A study of the immunology of the chronic fatigue syndrome: Correlation of immunologic markers to health dysfunction. Clinical Immunology & Immunopathology 87(1):60-67, 1998
- Peakman M, Deale A, Field R, Mahalingam M, Wessely S: Clinical improvement in chronic fatigue syndrome is not associated with lymphocyte subsets of function or activation. Clinical Immunology & Immunopathology 82(1):83-91, 1997
(i) Abnormally high or Low CD4/CD8 ratio and other T cell abnormalities
T-cell helper to T-cell suppressor ratio. Normal ratio for CD4 cell : CD8 cell is 1 : 4. Abnormal ratios suggests immune dysfunction. In ME this depends on :
(i)
the existence of subgroups
(ii)
the progression of the illness over time in phases (Hornig et al. (2013), Dr. Paul Cheney (3 phases of the illness)
(iii)
if the patient is having active infection(s) including opportunistic infections
(iv)
whether he/she is in remission or in relapse. And if they have mild, moderate or severe ME.
(iv) the patient's genetic weaknesses
(v) gradual onset ME or rapid onset ? .
- Abnormally High or Low CD4/CD8 ratio found in subsets of patients
"Patients had a higher mean (+/- SD) CD4/CD8 T-cell ratio than matched healthy controls (3.16 +/- 1.5 compared with 2.3 +/- 1.0, respectively; P < 0.003)."
Buchwald, D., Cheney, P., Peterson, D., Henry, B., Wormsley, S., Geiger, A., Ablashi, D., Komaroff, D.etc. 1992. A chronic illness characterized by fatigue, neurologic and immunologic disorders, and active Human Herpesvirus Type 6 Infection. Annals of Internal Medicine 1116: 103-13. (The seminal scientific research paper on the Lake Tahoe epidemic in the USA in the mid 1980's and the origin of the term CFS).
Get CD4 and CD8 cell counts. Normal ratio for CD4 cell : CD8 cell is 2 or 3. Test for abnormal ratio which suggests immune dysfunction.
Abnormal Low CD4/CD8 ratio found
in some studies
Klimas, N. G., F. R. Salvato, R. Morgan, and M. A. Fletcher. 1990. Immunologic abnormalities in chronic fatigue syndrome. J. Clin. Microbiol. 28:1403-1410
Levine, P. H., T. L. Whiteside, D. Friberg, J. Bryant, G. Colclough, and R. B. Herberman. 1998. Dysfunction of natural killer activity in a family with chronic fatigue syndrome. Clin. Immunol. Immunopathol. 88:96-104.
Straus, S. E., S. Fritz, J. K. Dale, B. Gould, and W. Strober. 1993. Lymphocyte phenotype and function in the chronic fatigue syndrome. J. Clin. Immunol. 13:30-40.
- CD8 is necessary to control latent viruses and other pathogens. The reduction of CD8's may be responsilbe for the reactivated latent viruses and pathogens in ME patients.
- Study of immune alterations in patients with chronic fatigue syndrome with different etiologies.Racciatti D, Dalessandro M, Delle Donne L, Falasca K, Zingariello P, Paganelli R, Pizzigallo E, Vecchiet J. Int J Immunopathol Pharmacol. 2004 May-Aug;17(2 Suppl):57-62.
- Straus SE, Tosato G, Armstrong G, et al: Persisting illness and fatigue in adults with evidence of Epstein-Barr virus infection. Ann Intern Med 102:7-16, 1985
- Buchwald D, Komaroff AL: Review of laboratory findings for patients with chronic fatigue syndrome. Rev Infect Dis 13(1):S12-S18, 1991
- Aoki T, Usuda Y, Miyakashi H, et al: Low natural syndrome: clinical and immunologic features. Nat Immun Cell Growth Regul 6:116-128, 1987
- DuBois RE: Gamma globulin therapy for chronic mononucleosis syndrome. AIDS Res Hum Retroviruses 2(1):S191-S195, 1986
- "A significant increase in Tregs was observed in both 1994 CDC
and ICC patients in comparison to healthy controls (Figure 2). Further,
a significant decrease in CD39
+
Tregs was observed in 1994 CDC
patients in comparison to healthy controls............ HNA2 (CD177
-
) were significantly increased in 1994 CDC patients while HNA2
(CD177
+
) were significantly reduced in ICC patients in comparison to
healthy controls (Figure 3). HNA5 was higher in 1994 CDC patients in
comparison to ICC patients."
Brenu et al.. Immune Abnormalities in Patients Meeting New Diagnostic Criteria for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis.J Mol Biomark Diagn 2013, 4:3 .
- Lloyd, A. R., D. Wakefield, C. R. Boughton, and J. M. Dwyer. 1989. Immunological abnormalities in the chronic fatigue syndrome. Med. J. Austral. 151:122-124.
- D. M., P. Cimoch, S. Chou, J. Chang, and J. Tilles. 1998. The in vitro immunomodulatory effects of glyconutrients on peripheral blood mononuclear cells of patients with chronic fatigue syndrome. Integr. Physiol. Behav. Sci. 33:280-287.
- Immunology Primer for Practitioners.
IACFS/ME Conference. Translating Science into Clinical Care. March 20-23, 2014 • San Francisco, California, USA
Daniel Peterson, M.D., Griffith University, Gold Coast, Australia, Owner, Sierra Internal Medicine, Incline Village, NV
Sonya Marshall - Gradisnik, BSc (Hons), Ph.D. , Professor of Immunology, Director, National Centre for Neuroimmunology & Emerging Diseases, Griffith University, Australia
Sharni Hardcastle, Ph.D., Research Assistant and Practical Demonstrator , Bond University, Gold Coast, Australia
Nancy Klimas, M.D. Ph.D., Professor of Medicine and Director, NSU COM Institute for Neuro-Immune Medicine Director, Miami VAMC Gulf War Illness and ME/CFS Research Program
Paula Waziry, Ph.D, Assistant Professor, Neuro Immune Medicine, COM, Nova Southeastern University, Miami, Fl
Konstance Knox, Ph.D., Founder, CEO, Coppe Healthcare Solutions
David Baewer, M.D. Ph.D, Medical Director, Coppe Healthcare Solutions
Isabel Barao, Ph.D., Research Assistant Professor, University of Nevada, Reno, Simmaron Research Scientific
Gunnar Gottschalk, B.S., Simmaron Research, Incline Village, NV
Troy Querec, Ph.D., Associate Service Fellow, Centers for Disease Control and Prevention, Atlanta, GA
Dennis Mangan, Ph.D., Chair, Trans-NIH ME/CFS Research Working Group, Office of Research on Women's Health, U.S. National Institutes of Health
Mary Ann Fletcher, Ph.D., University of Miami Miller School of Medicine Professor of Medicine, Microbiology/Immunology and Psychology
Elizabeth Unger, M.D. Ph.D., Chief, Chronic Viral Disease Branch, Division of High-Consequence Pathogens and Pathology, National Center for Emerging and Zoonotic Infectious Diseases. Centers for Disease Control and Prevention, Atlanta, GA
- Linde A, Hammarstrom L, Smith CIE: IgG subclass deficiency and chronic fatigue syndrome. Lancet 1:885-886, 1988
- Jones JF, Straus SE: Chronic Epstein-Barr virus infection. Annu Rev Med 38:195-209, 1987
- Jones JF, Ray G, Minnich LL, et al: Evidence for active Epstein-Barr virus infection in patients with persistent, unexplained illnesses: elevated anti-early antigen antibodies. Ann Intern Med 102:1-7, 1985
- Borysiewicz LK, Haworth SJ, Cohen J, et al: Epstein-Barr virus - specific immune defects in patients with persistent symptoms following infectious mononucleosis. Q J Med 58:111-121, 1986
- Sandman CA, Barron JL, Nackoul KA, Fidler PL, Goldstein J: Is there a chronic fatigue syndrome (CFS) dementia?
- Pukhal'ski
i
AL
,
Shmarina GV
,
Aleshkin VA
. Regulatory T-cells: modern approaches to
optimization of their numbers.
Vestn Ross Akad Med Nauk.
2011;(8):24-33. PMID:
21950132
- Kerr JR, Petty R, Burke B, Gough J, Fear D, Sinclair LI, et al. Gene expression
subtypes in patients with chronic fatigue syndrome/myalgic encephalomyelitis.
J Infect
Dis
(
2008
)
197
:
1171
-
1184.
- Hardcastle SL, Brenu EW, Johnston S, Nguyen T, Huth T, Kaur M, et al. Analysis of
the relationship between immune
dysfunction and symptom severity in patients with
Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (CFS/ME).
J Clin Cell Immunol
(
2014
)
5
:
190.
- T-cell subsets and phenotypes. "CFS diagnosed individuals showed similar absolute numbers of T, B and NK cells, with minor differences in the percentage of CD4+ and CD8+ T cells. B cells showed similar subset frequencies and proliferative responses between groups. Conversely, significant differences were observed in T cell subsets. CFS individuals showed increased levels of T regulatory cells (CD25+/FOXP3+) CD4 T cells, and lower proliferative responses in vitro and in vivo. Moreover, CD8 T cells from the CFS group showed significantly lower activation and frequency of effector memory cells. No clear signs of T-cell immunosenescence were observed."
"increase in the proportion of CD4 T-cells expressing the PD-1 (CD279) marker"
"CD8 T-cells expressing the CD5 marker were higher"
"lower counts of the activation marker CD38 and memory CD8 T-cells displaying the marker CD45RO."
Screening NK-, B- and T-cell phenotype and function in patients suffering from Chronic Fatigue Syndrome. Curriu et al. Journal of Translational Medicine 2013, 11:68
- "Much
of the Belgian research focused on the abnormal enzyme pathways and
88% of patients tested positive to RnaseL, (as found by Suhadolnik).
The 37Kda is produced by calpain cleavage, and the whole process
affects the calcium and potassium channel mechanisms. RnaseL is a
likely marker for CFS, and correlates with severity. (It is negative
in AIDS). The ALT and the haematocrit are adversely affected by the
abnormal RnaseL ratio and when the ratio is higher the serum calcium
is low, which is consistent with a channelopathy. The channelopathy
will lead to low body potassium because of loss, metabolic alkalosis
and hyperventilation syndrome. Symptoms relating to CVS, abnormal
hormone levels and abnormal exercise response follow. There is a
secondary hypomagnesia, abnormal sodium retention and changed
tryptophan uptake. The latter leads to depression. The CD4/CD8 ratio
correlates with VO2 max. A very complex model was proposed, the
mechanism leading to a Th1/Th2 shift with viral reactivation and
intracellular opportunistic infections. 68.7% patients were infected
with mycoplasma in Belgian studies with a predominance of M.hominis.
Mycoplasma can lead to calpain cleavage. Mycoplasma can invade all
tissues such as monocytes, muscle cells etc. "
K de Meirleir (Brussels), S Shetzline (Brussels), P Englebienne
(Brussels), P de Becker (Brussels), research papers submitted to the
AACFS 5th International Research, Clinical and Patient Conference,
2001
- "Compared to healthy individuals, CFS/ME patients displayed significant increases in IL-10, IFN-γ, TNF-α, CD4+CD25+ T cells, FoxP3 and VPACR2 expression. Cytotoxic activity of NK and CD8+T cells and NK phenotypes, in particular the CD56bright NK cells were significantly decreased in CFS/ME patients. Additionally granzyme A and granzyme K expression were reduced while expression levels of perforin were significantly increased in the CFS/ME population relative to the control population. These data suggest significant dysregulation of the immune system in CFS/ME patients.
Immunological abnormalities as potential biomarkers in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis Ekua W Brenu, Mieke L van Driel, Don R Staines, Kevin J Ashton, Sandra B Ramos, James Keane, Nancy G Klimas and Sonya M Marshall-Gradisnik. Journal of Translational Medicine 2011, 9:81 1)
- Chronic fatigue syndrome: clinical condition associated with immune activation.Landay AL, Jessop C, Lennette ET, Levy JA. Lancet. 1991 Sep 21;338(8769):707-12.
- CD8 subsets and markers
- ' In the CFS/ME patients CD127 was significantly decreased on all subsets of CD8+ T cells in comparison to the nonfatigued controls. PSGL-1 was significantly reduced in the CFS/ME patients in comparison to the nonfatigued controls.' J Immunol Res. 2016;2016:9064529. doi: 10.1155/2016/9064529. Epub 2016 Jan 4. A Preliminary Comparative Assessment of the Role of CD8+ T Cells in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis and Multiple Sclerosis. Brenu EW, Broadley S, Nguyen T, Johnston S, Ramos S, Staines D, Marshall-Gradisnik S.
- CD45RO increased
Straus, S. E., S. Fritz, J. K. Dale, B. Gould, and W. Strober. 1993. Lymphocyte phenotype and function in the chronic fatigue syndrome. J. Clin. Immunol. 13:30-40.
- A reduced CD8 suppressor cell population and increased activation markers (CD38, HLA-DR) on CD8 cells were found.
Landay, A. L., C. Jessop, E. T. Lennette, and J. A. Levy. 1991. Chronic fatigue syndrome: clinical condition associated with immune activation. Lancet 338:707-712.
Klimas, N. G., F. R. Salvato, R. Morgan, and M. A. Fletcher. 1990. Immunologic abnormalities in chronic fatigue syndrome. J. Clin. Microbiol. 28:1403-1410.
Lloyd, A. R., D. Wakefield, C. R. Boughton, and J. M. Dwyer. 1989. Immunological abnormalities in the chronic fatigue syndrome. Med. J. Austral. 151:122-124.
- Barker E, Fujimura SF, Fadem MB, Landay AL, Levy JA: Immunologic abnormalities associated with chronic fatigue syndrome. Clin Infect Dis 18(supp 1):S136-S141, 1994
- HLA DR abnormalities. Chronic fatigue syndrome: clinical condition associated with immune activation. A.L. Landay, E.T. Lennette, C. Jessop, J.A. Levy. The Lancet, Volume 338, Issue 8769, 21 September 1991, Pages 707-712.
- Straus, S. E., S. Fritz, J. K. Dale, B. Gould, and W. Strober. 1993. Lymphocyte phenotype and function in the chronic fatigue syndrome. J. Clin. Immunol. 13:30-40.
- Lusso,
P. et al.; "Productive Infection of CD4-Positive and CD8-Positive
Mature Human T Cell Populations and Clones by Human Herpesvirus
6"; Journal of Immunology 147(2):685, July 15, 1991.
- Prieto, J., M. L. Subira, A. Castilla, and M. Serrano. 1989. Naloxone-reversible monocyte dysfunction in patients with chronic fatigue syndrome. Scand. J. Immunol. 30:13-20.
- Lloyd, A. R., D. Wakefield, C. R. Boughton, and J. M. Dwyer. 1989. Immunological abnormalities in the chronic fatigue syndrome. Med. J. Austral. 151:122-124.
- Chao, C. C., E. N. Janoff, S. Hu, K. Thomas, M. Gallagher, M. Tsang, and P. K. Peterson. 1991. Altered cytokine release in peripheral blood mononuclear cell cultures from patients with the chronic fatigue syndrome. Cytokine 3:292-298.
- T reg cell exhaustion
- Jones JF, Straus SE: Chronic Epstein-Barr virus infection. Annu Rev Med 1987, 38:195-209.
- Borysiewicz LK, Haworth SJ, Cohen J, Mundin J, Rickinson A, Sissons JG: Epstein-Barr virus - specific immune defects in patients with persistent symptoms following infectious mononucleosis. Q J Med 1986, 58:111-121.
- Klimas N, Salvato F, Morgan R, Fletcher MA: Immunologic abnormalities in chronic fatigue syndrome. J Clin Microbiol 1990, 28:1403-1410.
- Behan PO, Behan WHM, Bell EJ: The postviral fatigue syndrome - an analysis of the findings in 50 cases. J Infect 1985, 10:211-222.
- Tobi M, Morag A, Ravid Z, Chowers I, Feldman-Weiss V, Michaeli Y, Ben-Chetrit E, Shalit M, Knobler H: Prolonged atypical illness associated with serological evidence of persistent Epstein-Barr infection. Lancet 1982, 1:61-64.
- The Dubbo Studies which were published in leading medical journals point to genetic factors, environmental factors and a post-infectious dysfunctional immune system as being the key factors in ME / CFS.
Post-infective and chronic fatigue syndromes precipitated by viral and non-viral pathogens: prospective cohort study. Hickie I, Davenport T, Wakefield D, Vollmer-Conna U, Cameron B, Vernon SD, Reeves WC, Lloyd A; Dubbo Infection Outcomes Study Group.
BMJ. 2006 Sep 16;333(7568):575. Epub 2006 Sep 1.
Cytokine polymorphisms have a synergistic effect on severity of the acute sickness response to infection.
Vollmer-Conna U, Piraino BF, Cameron B, Davenport T, Hickie I, Wakefield D, Lloyd AR; Dubbo Infection Outcomes Study Group.
Clin Infect Dis. 2008 Dec 1;47(11):1418-25. doi: 10.1086/592967
.
(i) Immunoglobulins
Abnormal low levels of IgG1, 2 and 3 in subgroups
- Decreased amounts of of the G, A, M, or D classes (Review: Immunology of Chronic Fatigue Syndrome Roberto Patarca, Timothy Mark, Mary Ann Fletcher and Nancy Klimas)
- Reduced IgG subclass 1 and 3. This suggests infection and lowered ability to fight active infections and control latent infections.
IgG, Immune complex, and Atypical Lymphocyte count abnormalities. Bates DW et al. Arch Intern Med 1995; 155: 97. (10 year study).
- IgM-related immune response directed against neopitopes.
Maes M, Mihaylova I, Leunis JC: Chronic fatigue syndrome is accompanied by an IgM-related immune response directed against neopitopes formed by oxidative or nitrosative damage to lipids and proteins. Neuro Endocrinol Lett 2006, 27:615-621
- Polyclonal immunoglobulin was elevated in 25% of patients and there was evidence for immunodeficiency in a further 25%. There was MBL deficiency in 15% (and 7% in controls) making these patients more prone to infection.
(Invest in ME Scientific Conference, 2013 Professor Carmen Scheibenbogen, Berlin,Germany)
- Patarca, R. (2001), Cytokines and Chronic Fatigue Syndrome. Annals of the New York Academy of Sciences, 933: 185–200. doi: 10.1111/j.1749-6632.2001.tb05824.x
- Wakefield, D., A. Lloyd, and A. Brockman. 1990. Immunoglobulin subclass abnormalities in patients with chronic fatigue syndrome. Pediatr. Infect. Dis. J. 9(Suppl.):S50-S53.
- Lloyd, A. R., D. Wakefield, C. R. Boughton, and J. M. Dwyer. 1989. Immunological abnormalities in the chronic fatigue syndrome. Med. J. Austral. 151:122-124.
- Natelson, B. H., J. J. LaManca, T. Denny, A. C. Vladutiu, J. Oleske, M. Hill, M. T. Bergen, L. Korn, and J. Hay. 1998. Immunological parameters in chronic fatigue syndrome, major depression, and multiple sclerosis. Am. J. Med. 105:43S-49S.
(j) Immune Complement activity, Endorphins, Monocytes, Weakened immune response and other Immune system abnormalities
- Serpin - Upregulation of Serpin in ME patients. This is important in the context of viral infection, immune dysfunction, RnaseL abnormality and elastase activity (Findings of Hornig et al., September 2013).
- Liu DH, Liu ZD, Li YZ, Zhang HY, Hu CJ, Zhang YB, Whang DX: Expression of lymphocyte subsets and CD25 ~ + regulative T Cells in peripheral blood of patients with chronic fatigue syndrome. Labeled Immunoassays and Clinical Medicine. Abstract 2011, 2011–02.
- Murdoch,
J. Campbell; "Cell Mediated Immunity in Patients With Myalgic
Encephalomyelitis Syndrome"; New Zealand Medical Journal, p.
511, August 10, 1988.
- Role of Infection and Neurologic Dysfunction in Chronic Fatigue Syndrome. Anthony L. Komaroff Tracey A. Cho. Semin Neurol 2011; 31(3): 325-337
- Bates, D. W., D. Buchwald, J. Lee, P. Kith, T. Doolittle, C. Rutherford, W. H. Churchill, P. H. Schur, M. Wener, D. Wybenga, J. Winkelman, and A. L. Komaroff. 1995. Clinical laboratory test findings in patients with chronic fatigue syndrome. Arch. Intern. Med. 155:97-103.
- Ziegler SF, Buckner JH: FOXP3 and the regulation of Treg/Th17 differentiation. Microbes Infect 2009, 11:594-598.
- Popmihajlov Z, Smith KA: Negative feedback regulation of T cells via interleukin-2 and FOXP3 reciprocity. PLoS ONE 2008, 3:e1581.
- Aspler AL, Bolshin C, Vernon SD, Broderick G (2008) Evidence of inflammatory immune signaling in chronic fatigue syndrome: A pilot study of gene expression in peripheral blood. Behav Brain Funct 4: 44
- Klimas N, Koneru AO: Chronic fatigue syndrome: inflammation, immune function, and neuroendocrine interactions. Curr Rheumatol Rep 2007, 9:482-487.
- BrunetJL,LiaudetAP,LaterR,etal.Delayed-typehypersensitivityandchronicfatiguesyndrome:theusefulnessofassessingT-cellactivationbyflowcytometry—preliminarystudy.AllergImmunol(Paris).2001;33:166–72.
-
Capelli E, Zola R, Lorusso L, Venturini L, Sardi F, Ricevuti G: Chronic fatigue syndrome/myalgic encephalomyelitis: an update. Int J Immunopathol Pharmacol 2010, 23:981-989.
- Jason LA, Sorenson M, Porter N, Belkairous N (2010), "An Etiological Model for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome", Neuroscience & Medicine, 2011, 2, 14-27, PMID: 21892413
- Loebel M, Strohschein K, Giannini C, Koelsch U, Bauer S, Doebis C, Thomas S, Unterwalder N, Von Baehr V, Reinke P, Knops M, Hanitsch LG, Meisel C, Volk H-D, Scheibenbogen C (2014), "Deficient EBV-Specific B- and T-Cell Response in Patients with Chronic Fatigue Syndrome", PLoS ONE 9(1): e85387.
- The Dubbo Studies which were published in leading medical journals point to genetic factors, environmental factors and a post-infectious dysfunctional immune system as being the key factors in ME / CFS.
Post-infective and chronic fatigue syndromes precipitated by viral and non-viral pathogens: prospective cohort study. Hickie I, Davenport T, Wakefield D, Vollmer-Conna U, Cameron B, Vernon SD, Reeves WC, Lloyd A; Dubbo Infection Outcomes Study Group.
BMJ. 2006 Sep 16;333(7568):575. Epub 2006 Sep 1.
Cytokine polymorphisms have a synergistic effect on severity of the acute sickness response to infection.
Vollmer-Conna U, Piraino BF, Cameron B, Davenport T, Hickie I, Wakefield D, Lloyd AR; Dubbo Infection Outcomes Study Group.
Clin Infect Dis. 2008 Dec 1;47(11):1418-25. doi: 10.1086/592967.
- Immune Abnormalities in Patients Meeting New Diagnostic Criteria for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis.J Mol Biomark Diagn 2013, 4:3
- Beta Endorphins
- Decreased immunoreactive beta-endorphin in mononuclear leucocytes from patients with chronic fatigue syndrome. Conti F, Pittoni V, Sacerdote P, Priori R, Meroni PL, Valesini G. Clin Exp Rheumatol. 1998 Nov-Dec;16(6):729-32.
- Peripheral blood mononuclear cell beta-endorphin concentration is decreased in chronic fatigue syndrome and fibromyalgia but not in depression: preliminary report. Panerai AE, Vecchiet J, Panzeri P, Meroni P, Scarone S, Pizzigallo E, Giamberardino MA, Sacerdote P. Clin J Pain. 2002 Jul-Aug;18(4):270-3.
- Bates DW et al. Arch Intern Med 1995; 155: 97. (10 year study) .IgG, Immune complex, and Atypical Lymphocyte count abnormalities.
- Evidence for inflammation and activation of cell-mediated immunity in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): Increased interleukin-1, tumor necrosis factor-α, PMN-elastase, lysozyme and neopterin. Michael Maes et al. Journal of Affective Disorders Volume 136, Issue 3, February 2012, Pages 933–939
- Immunology Primer for Practitioners.
IACFS/ME Conference. Translating Science into Clinical Care. March 20-23, 2014 • San Francisco, California, USA
Daniel Peterson, M.D., Griffith University, Gold Coast, Australia, Owner, Sierra Internal Medicine, Incline Village, NV
Sonya Marshall - Gradisnik, BSc (Hons), Ph.D. , Professor of Immunology, Director, National Centre for Neuroimmunology & Emerging Diseases, Griffith University, Australia
Sharni Hardcastle, Ph.D., Research Assistant and Practical Demonstrator , Bond University, Gold Coast, Australia
Nancy Klimas, M.D. Ph.D., Professor of Medicine and Director, NSU COM Institute for Neuro-Immune Medicine Director, Miami VAMC Gulf War Illness and ME/CFS Research Program
Paula Waziry, Ph.D, Assistant Professor, Neuro Immune Medicine, COM, Nova Southeastern University, Miami, Fl
Konstance Knox, Ph.D., Founder, CEO, Coppe Healthcare Solutions
David Baewer, M.D. Ph.D, Medical Director, Coppe Healthcare Solutions
Isabel Barao, Ph.D., Research Assistant Professor, University of Nevada, Reno, Simmaron Research Scientific
Gunnar Gottschalk, B.S., Simmaron Research, Incline Village, NV
Troy Querec, Ph.D., Associate Service Fellow, Centers for Disease Control and Prevention, Atlanta, GA
Dennis Mangan, Ph.D., Chair, Trans-NIH ME/CFS Research Working Group, Office of Research on Women's Health, U.S. National Institutes of Health
Mary Ann Fletcher, Ph.D., University of Miami Miller School of Medicine Professor of Medicine, Microbiology/Immunology and Psychology
Elizabeth Unger, M.D. Ph.D., Chief, Chronic Viral Disease Branch, Division of High-Consequence Pathogens and Pathology, National Center for Emerging and Zoonotic Infectious Diseases. Centers for Disease Control and Prevention, Atlanta, GA
- Host response to infection. Including post-infection phase.
Hickie I, et al. Post-infective and chronic fatigue syndromes precipitated by viral and non-viral pathogens: prospective cohort study. British Journal of Medicine 2006; 333 (7568):575.
- T-cell subsets and phenotypes. "CFS diagnosed individuals showed similar absolute numbers of T, B and NK cells, with minor differences in the percentage of CD4+ and CD8+ T cells. B cells showed similar subset frequencies and proliferative responses between groups. Conversely, significant differences were observed in T cell subsets. CFS individuals showed increased levels of T regulatory cells (CD25+/FOXP3+) CD4 T cells, and lower proliferative responses in vitro and in vivo. Moreover, CD8 T cells from the CFS group showed significantly lower activation and frequency of effector memory cells. No clear signs of T-cell immunosenescence were observed."
"increase in the proportion of CD4 T-cells expressing the PD-1 (CD279) marker"
"CD8 T-cells expressing the CD5 marker were higher"
"lower counts of the activation marker CD38 and memory CD8 T-cells displaying the marker CD45RO."
Screening NK-, B- and T-cell phenotype and function in patients suffering from Chronic Fatigue Syndrome. Curriu et al. Journal of Translational Medicine 2013, 11:68
- FOXP3 Upregulation. Invest in ME Scientific Conference 2012, 2013.
- Bates, D. W., D. Buchwald, J. Lee, P. Kith, T. Doolittle, C. Rutherford, W. H. Churchill, P. H. Schur, M. Wener, D. Wybenga, J. Winkelman, and A. L. Komaroff. 1995. Clinical laboratory test findings in patients with chronic fatigue syndrome. Arch. Intern. Med. 155:97-103.
- Prieto, J., M. L. Subira, A. Castilla, and M. Serrano. 1989. Naloxone-reversible monocyte dysfunction in patients with chronic fatigue syndrome. Scand. J. Immunol. 30:13-20.
- Maher KJ, Klimas NG, Fletcher MA: Chronic fatigue syndrome is associated with diminished intracellular perforin. Clin Exp Immunol 2005, 142:505-511.
- Meeus M, Mistiaen W, Lambrecht L, Nijs J (2009), "Immunological similarities between cancer and chronic fatigue syndrome: the common link to fatigue?", Anticancer Res, Nov;29(11):4717-26, PMID: 20032425,
- Lutgendorf S, Klimas NG, Antoni M, Brickman A, Fletcher MA: Relationships of cognitive difficulties to immune measures, depression and illness burden in chronic fatigue syndrome. Journal of Chronic Fatigue Syndrome 1(2):23-41, 1995
- "Although
serum immunoreactivity to BDV proteins observed
in Swedish CFS patients by ELISA may reflect
infection with related microbial agents that induce
cross-reactivity with conformational determinants
on BDV proteins (Kliche
et al
, 1996) and
b
-
galactosidase, the serologic findings are also consistent with non specific polyclonal B-cell activation."
Absence of evidence of Borna disease virus infection in Swedish patients with Chronic Fatigue Syndrome Birgitte Evenga╩rd,
Thomas Briese
, Gudrun Lindh
, Shaun Lee
and W Ian Lipkin
- Hardcastle SL, Brenu EW, Johnston S, Nguyen T, Huth T, Kaur M, et al. Analysis of
the relationship between immune
dysfunction and symptom severity in patients with
Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (CFS/ME).
J Clin Cell Immunol
(
2014
)
5
:
190.
- Elevated CD26 levels. "Percent CD2+ lymphocytes (T cells and NK cells) positive for DPPIV/C26 was elevated in CFS cases, but there was a decrease in the number of molecules (rMol) of DPPIV/C26 expressed on T cells and NK cells and a decrease in the soluble form of the enzyme in serum." ( Biomarkers in Chronic Fatigue Syndrome: Evaluation of Natural Killer Cell Function and Dipeptidyl Peptidase IV/CD26 Mary A. Fletcher et al. PLoS One. 2010 )
- CD69 marker. "The expression of the CD69 activation marker on T cells (CD3+, CD3+CD4+, and CD3+CD8+) and on NK cells (CD45+CD56+) was significantly lower in CFS patients than in healthy subjects. These differences were significant to the extent that a significant diagnostic performance was obtained, i.e. the area under the ROC curve was around 89%. No differences either in the number of leukocytes or in the number or percentage of lymphocytes, i.e. CD3, CD4, CD8 and CD19, could be found between CFS patients and the controls. Patients with CFS show defects in T- and NK cell activation."
Decreased expression of CD69 in chronic fatigue syndrome in relation to inflammatory markers: evidence for a severe disorder in the early activation of T lymphocytes and natural killer cells. Mihaylova I, DeRuyter M, Rummens JL, Bosmans E, Maes M.. Neuro Endocrinol Lett. 2007 Aug;28(4):477-83.
- Decrease in neutrophil respiratory bursts. Neutrophil antigens HNA-2 and HNA-5 are abnormal. Invest in ME Scientific Conference, 2012, 2013 (Dr. Donald Staines).
- Elevated levels of Immune Complexes
Straus SE, Tosato G, Armstrong G, et al: Persisting illness and fatigue in adults with evidence of Epstein-Barr virus infection. Ann Intern Med 102:7-16, 1985
Borysiewicz LK, Haworth SJ, Cohen J, et al: Epstein-Barr virus - specific immune defects in patients with persistent symptoms following infectious mononucleosis. Q J Med 58:111-121, 1986
Behan PO, Behan WHM, Bell EJ: The postviral fatigue syndrome - An analysis of the findings in 50 cases. J Infect 1985;10:211-22, 1985
Bates DW, Buchwald D, Lee J, Kith P, Doolittle T, Rutherford C, Churchill WH, Schur PH, Werner M, Wybenga D, et al: Clinical laboratory test findings in patients with chronic fatigue syndrome. Arch of Intern Med 155:97-103, 1995
- Maes M, Mihaylova I, Leunis JC: Chronic fatigue syndrome is accompanied by an IgM-related immune response directed against neopitopes formed by oxidative or nitrosative damage to lipids and proteins. Neuro Endocrinol Lett 2006, 27:615-621
- Okadaic acid-like toxin in systemic lupus erythematosus patients: hypothesis for toxin-induced pathology, immune dysregulation, and transactivation of herpesviruses; Mitchell TM; Med Hypotheses. 1996 Sep;47(3):217-25. Herpes virus infections are of interest to ME / CFS patients and research.
- Elevated Eosinophil levels in ME patients who have illness for 3 years or less. (Findings of Hornig et al., September 2013)
- Kavelaars A
,
Kuis W
,
Knook L
,
Sinnema G
,
Heijnen CJ
. Disturbed neuroendocrine-
immune interactions in chronic fatigue syndrome.
J Clin Endocrinol Metab.
2000 Feb;85
(2):692-6. PMID: 10690878
- Elevated Serum IL-1, TNFα, neopterin and lysozyme levels. "Serum IL-1, TNFα, neopterin and lysozyme are significantly higher in patients with ME/CFS than in controls" ( Evidence for inflammation and activation of cell-mediated immunity in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): Increased interleukin-1, tumor necrosis factor-α, PMN-elastase, lysozyme and neopterin. Michael Maes et al. Journal of Affective Disorders Volume 136, Issue 3, February 2012, Pages 933–939 )
-
In
the book 'Oslers web' the scientific findings showed abnormally high
T-cell helper to T-cell suppressor ratios. Some patients hade ratios of over 5:1, and 10:1. Oslers Web, by Hillary Johnson, Penguin Books 1997, page 95. Int J Immunopathol Pharmacol. 2004 May-Aug;17(2 Suppl):57-62.
- Lymphopenia in a subset of patients (Invest in ME Scientific Conference, 2013 Professor Carmen Scheibenbogen, Berlin,Germany)
- I. J. Elenkov, R.L. Wilder, G. P. Chrousos and E. S. Vizi, "The Sympathetic Nerve—An Integrative Interface Between Two Supersystems: The Brain and the Immune System," Pharmacological Reviews, Vol. 52, No. 2, 2000, pp. 595-638.
- Kerr JR, Petty R, Burke B, Gough J, Fear D, Sinclair LI, et al. Gene expression
subtypes in patients with chronic fatigue syndrome/myalgic encephalomyelitis.
J Infect
Dis
(
2008
)
197
:
1171
-
1184.
- Polyclonal immunoglobulin was elevated in 25% of patients and there was evidence for immunodeficiency in a further 25%. There was MBL deficiency in 15% (and 7% in controls) making these patients more prone to infection.
(Invest in ME Scientific Conference, 2013 Professor Carmen Scheibenbogen, Berlin,Germany)
- Study of immune alterations in patients with chronic fatigue syndrome with different etiologies.Racciatti D, Dalessandro M, Delle Donne L, Falasca K, Zingariello P, Paganelli R, Pizzigallo E, Vecchiet J. Int J Immunopathol Pharmacol. 2004 May-Aug;17(2 Suppl):57-62.
- CD8 lysis reduced and high levels of HNA2 (Invest in ME Scientific Conference, 2012, 2013 (Dr. Donald Staines)
- mRNA CD8 cells show consistent abnormalities (Invest in ME Scientific Conference, 2012, 2013 (Dr. Donald Staines)
- Drexhage R (2011), "Immuno-neuro-endocrine networks. A study on the inflammatory state of circulating monocytes and CD4+ T cells in psychiatric and endocrine autoimmune disease" (proefschrift), Erasmus MC, Rotterdam, ISBN: 978-90-5335-405-6
- Hassan IS, Bannister BA, Akbar A, Weir W, Bofill M: A study of the immunology of the chronic fatigue syndrome: Correlation of immunologic markers to health dysfunction. Clinical Immunology & Immunopathology 87(1):60-67, 1998
- Behan PO, Behan WHM, Bell EJ: The postviral fatigue syndrome - An analysis of the findings in 50 cases. J Infect 1985;10:211-22, 1985
- Oxidative and Nitrosative Stress and Immune-Inflammatory Pathways in Patients with Myalgic Encephalomyelitis (ME)/Chronic Fatigue Syndrome (CFS). Maes et al. Curr Neuropharmacol. 2014 Mar;12(2):168-85.
- Tobi M, Morag A, Ravid Z, et al: Prolonged atypical illness associated with serological evidence of persistent Epstein-Barr infection. Lancet 1:61-64, 1982
- Subira ML, Castilla A, Civeira MP, et al: Deficient display of CD3 on lymphocytes of patients with chronic fatigue syndrome. J Infect Dis 160:165-166, 1989
- Immunological abnormalities as potential biomarkers in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis
Ekua W Brenu1,2, Mieke L van Driel, Don R Staines, Kevin J Ashton, Sandra B Ramos, James Keane, Nancy G Klimas, Sonya M Marshall-Gradisnik. Journal of Translational Medicine 2011, 9:81. (2011)
- Cameron B, Bharadwaj M, Burrows J, Fazou C, Wakefield D, Hickie I, Ffrench R, Khanna R, Lloyd A (2006), "Prolonged Illness after Infectious Mononucleosis Is Associated with Altered Immunity but Not with Increased Viral Load", JID 193 (1 March):664-671
- Acheson ED (1956), "A New Clinical Entity?", Leading Article, Lancet, 26 mei, pp. 789-90
- Acheson ED (1959), "The clinical syndrome variously called benign myalgic encephalomyelitis, Iceland disease, and epidemic neuromyasthenia", Am J Med Apr;26(4):569-95, PMID: 13637100
- Chronic fatigue syndrome: clinical condition associated with immune activation.Landay AL, Jessop C, Lennette ET, Levy JA. Lancet. 1991 Sep 21;338(8769):707-12.
- Hanson SJ, et al. Detection of immunologically significant factors for chronic fatigue syndrome using neural-network classifiers. Clin Diagn Lab Immunol 2001;8:658-62.
- Demettre E, et al. Ribonuclease L proteolysis in peripheral blood mononuclear cells of chronic fatigue syndrome patients. J Biol Chem 2002;277(38):35746.
- Lapp, Charles W. "Chronic Fatigue is a real disease". North Carolina Family Physician 43:1 (Winter 1992). Main finding - High levels of Interleukin 1 and 2.
- Increased neutrophil apoptosis in chronic fatigue syndrome. Kennedy G, Spence V, Underwood C, Belch JJ; J Clin Pathol 2004:57(8):891-893
- Vojdani A, Ghoneum M, Choppa PC, Magtoto L, Lapp CW: Elevated apoptotic cell population in patients with chronic fatigue syndrome: The pivotal role of protein kinase RNA. Journal of Internal Medicine 242(6):465-478, 1997
- A Chronic Illness Characterized by Fatigue, Neurologic and Immunologic Disorders, and Active Human Herpesvirus Type 6 Infection. Dedra Buchwald, MD; Paul R. Cheney, MD, PhD; Daniel L. Peterson, MD; Berch Henry, PhD; Susan B. Wormsley, BS; Ann Geiger, BA; Dharam V. Ablashi, DVM; S. Zaki Salahuddin, MS; Carl Saxinger, PhD; Royce Biddle, MD; Ron Kikinis, MD; Ferenc A. Jolesz, MD; Thomas Folks, PhD; N. Balachandran, PhD; James B. Peter, MD, PhD; Robert C. Gallo, MD; and Anthony L. Komaroff, MD. Ann Intern Med. 15 January 1992;116(2):103-113
- "
T cell function has been well studied in CFS. Thirteen published
studies have described abnormally low responses to T cell stimulation
in vitro. Two separate studies related the severity of T cell function
abnormality to the severity of symptoms and to the severity of
cognition. A "provocative study" suggests that T cells of
CFS patients do not express CD3 receptor. An important function of the
CD3 receptor is that it activates cells, which may explain the poor
response to antigens."
SOS (State of the Science) Conference
State of the Science Conference at the National Institutes of Health:
October 23-24, 2000
By Jill McLaughlin, National CFIDS Foundation, USA.
- Biochemical and Vascular Aspects of Pediatric Chronic Fatigue Syndrome
Gwen Kennedy, PhD; Faisel Khan, PhD; Alexander Hill, PhD; Christine Underwood, MBBS; Jill J. F. Belch, MD. Arch Pediatr Adolesc Med. 2010;164(9):817-823. doi:10.1001/archpediatrics.2010.157.
- Moderate exercise increases expression for sensory, adrenergic and immune genes in chronic fatigue syndrome patients, but not in normal subjects. Alan R. Light, Andrea T. White, Ronald W. Hughen, and Kathleen C. Light
- "If
you look at the T cell population, there are marked elevations of CD26
in majority of CFS patients. Also the elevation of T cell activation
markers in CFS correspond to severity of symptoms."
SOS (State of the Science) Conference
State of the Science Conference at the National Institutes of Health:
October 23-24, 2000
By Jill McLaughlin, National CFIDS Foundation, USA
-
CD4
T lymphocytes from patients with chronic fatigue syndrome have
decreased interferon-gamma production and increased sensitivity to
dexamethasone.Visser J; Blauw B; Hinloopen B; Brommer E; de Kloet ER;
Kluft C; Nagelkerken L; J Infect Dis 1998 Feb;177(2):451-4
-
Severe
Immune deficiencies found in CFS patients using Multitest.
Oslers Web, by Hillary Johnson, Penguin Books 1997, page 327
-
Landay
AL et al. Lancet 1991; 338: 707
-
Straus,
Stephen E. et al.; "Lymphocyte Phenotype and Function in the
Chronic Fatigue Syndrome"; Journal of Clinical Immunology
13(1):30, 1993.
-
Lloyd
A et al. Clin Exp Immunol 1992; 87: 786
-
Straus
SE, Dale JK, Wright R, and Metcalfe DD: Allergy and the Chronic
Fatigue Syndrome. J Allergy Clin Immunol 1988; 81:791--795
-
Jamal
GA and Hansen S: Post-Viral Fatigue Syndrome: Evidence for Underlying
Organic Disturbance in the Muscle Fiber. Eur Neurol 1989; 29:273--276
-
Peripheral
Blood Mononuclear Cell beta-Endorphin Concentration Is Decreased in
Chronic Fatigue Syndrome and Fibromyalgia but Not in Depression:
Preliminary Report
by Panerai AE, Vecchiet J, Panzeri P, Meroni P, Scarone S, Pizzigallo
E, Giamberardino MA, Sacerdote P. Clin J Pain 2002
Jul-Aug;18(4):270-273
-
Gin
W, Christiansen FT, Peter JB. Immune function and chronic fatigue
syndrome. Med J Aust 1989:151:117-8.
-
Gold
D, Bowden R, Sixbey J, Riggs R, Katon WJ, Ashley R, Obrigewitch RM,
and Corey L: Chronic Fatigue: a prospective clinical and virologic
study. J Am Med Assn 1990; 264:48--53
-
Buchwald
D: Fibromyalgia and Chronic Fatigue Syndrome: similarities and
differences. Rheum Dis Clin N A 1996; 22:219--243
- Nijs J, De Becker P, De Meirleir K, et al. Associations between bronchial hyperresponsiveness and immune cell parameters in patients with chronic fatigue syndrome.Chest.2003; 123:998–1007
- Chao
CC, Gallagher M, Phair J, and Peterson PK: Serum Neopterin and
Interleukin-6 Levels in Chronic Fatigue Syndrome. J Infectious Dis
1990; 162:1412--1413
-
Dynamics
of Chronic Active Herpesvirus-6 Infection in Patients with Chronic
Fatigue Syndrome: Data Acquisition for Computer Modeling
FibromyalgiaSupport.com
04-02-2002
Journal: In Vivo 2001 Nov-Dec;15(6):461-5
Authors: Krueger GR, Koch B, Hoffmann A, Rojo J, Brandt ME, Wang G,
Buja LM.
-
Grufferman,
S. et al.; "Epidemiologic Investigation of an Outbreak of Chronic
Fatigue-Immune Dysfunction Syndrome in a Defined Population";
American Journal of Epidemiology 128(4), 1988.
-
Roberto
Patarca, Timothy Mark, Mary Ann Fletcher and Nancy Klimas
Review: Immunology of Chronic Fatigue Syndrome
Journal of Chronic Fatigue Syndrome 2000; 6(3/4): 69-107.
-
Gupta,
S. and B. Vayavegula; "A Comprehensive Immunological Analysis in
Chronic Fatigue Syndrome"; Scandanavian Journal of Immunology
33:319, 1991
-
Hyde,
Byron Marshall, Editor; The Clinical and Scientific Basis of Myalgic
Encephalomyelitis/Chronic Fatigue Syndrome; Nightingale Research
Foundation, Ottawa, Ontario, Canada, 1992.
-
Lo,
Shyh-Ching et al.; "Association of the Virus-Like Infectious
Agent Originally Reported in Patients With AIDS With Acute Fatal
Disease in Previously Healthy Non-AIDS Patients"; Journal of
Tropical Medicine and Hygiene 41:364, 1989.
- Straus SE, Tosato G, Armstrong G, et al: Persisting illness and fatigue in adults with evidence of Epstein-Barr virus infection. Ann Intern Med 102:7-16, 1985
- Jones J: Serologic and immunologic responses in chronic fatigue syndrome with emphasis on the Epstein-Barr virus. Rev Infect Dis 13(1):S26-S31, 1991
- Jones JF, Straus SE: Chronic Epstein-Barr virus infection. Annu Rev Med 38:195-209, 1987
- Jones JF, Ray G, Minnich LL, et al: Evidence for active Epstein-Barr virus infection in patients with persistent, unexplained illnesses: elevated anti-early antigen antibodies. Ann Intern Med 102:1-7, 1985
- Borysiewicz LK, Haworth SJ, Cohen J, et al: Epstein-Barr virus - specific immune defects in patients with persistent symptoms following infectious mononucleosis. Q J Med 58:111-121, 1986
- Klimas
NG, Salvato FR, Morgan R, and Fletcher MA: Immunologic Abnormalities
in Chronic Fatigue Syndrome. J Clin Microbiol 1990; 28:1403--1410
- Gin
W, Christiansen FT, and Peter JB: Immune Function and the Chronic
Fatigue Syndrome. Med J Australia 1989; 151:117--118
- Elfaitouri A, Herrmann B, Bölin-Wiener A, Wang Y, Gottfries C-G, et al. (2013) Epitopes of Microbial and Human Heat Shock Protein 60 and Their Recognition in Myalgic Encephalomyelitis. PLoS ONE 8(11): e81155.
- Lloyd
A, Wakefield D, Boughton CR, and Dwyer JM: Immunological Abnormalities
in the Chronic Fatigue Syndrome. Med J Australia 1989; 151:122--124
- Straus
SE, Dale JK, Wright R, and Metcalfe DD: Allergy and the Chronic
Fatigue Syndrome. J Allergy Clin Immunol 1988; 81:791--795
- Lloyd A, Hickie I, Hickie C, Dwyer J, Wakefield D: Cell-mediated immunity in patients with chronic fatigue syndrome, healthy controls and patients with major depression. Clin exp Immunol 87(1):76-79, 1992
- Lloyd AR, Wakefield D, Boughton CR, et al: Immunological abnormalities in the chronic fatigue syndrome. Med J Aust 151:122-124, 1989
- Klimas N, Salvato F, Morgan R, Fletcher MA: Immunologic abnormalities in chronic fatigue syndrome. J Clin Microbiol 28(6):1403-1410, 1990
- Barker E, Fujimura SF, Fadem MB, Landay AL, Levy JA: Immunologic abnormalities associated with chronic fatigue syndrome. Clin Infect Dis 18(supp 1):S136-S141, 1994
- Aoki T, Usuda Y, Miyakashi H, et al: Low natural syndrome: clinical and immunologic features. Nat Immun Cell Growth Regul 6:116-128, 1987
- "there
is a growing body of research reporting distinguishing findings, such
as low level circulating immune complexes, elevated total complement,
increased activated CD8 cells, elevated IgG, atypical lymphocytes,
poorly functioning NK cells, low level ANA and abnormalities in the
RNaseL pathway"
"Professor Komaroff concluded that in view of the above evidence,
CFS has an organic basis, and in many of the patients there are
abnormalities of the limbic system in the brain and abnormal
regulation of the immune system, which is possibly a result of limbic
system abnormalities. A single cause seems unlikely, but multiple
triggering agents (infections, toxins, stress) could be
involved."
Research findings presented by Professor Anthony Komaroff (Boston,
Mass) to The Sydney ME / CFS Clinical and Scientific Conference,
December 2001
-
"Pathophysiological
mechanisms and CFS were discussed by Kenny de Meirleir (Brussels,
Belgium). He described this condition as having no single aetiologic
agent, but there are a number of predisposing factors leading to
abnormalities in the immune system. Viral reactivation and
opportunistic infections increase. Resultant ankyrin fragments from
pathologically cleaved RNaseL interact with ABC transporters, which
become dysfunctional, leading to many of the symptoms of CFS. This is
described as an acquired channelopathy. 206 CFS patients were studied
and 70% were found to be Mycoplasma positive, and these patients had
significantly more cleavage fragments of RNaseL.
He also mentioned the Bijlmer incident, when following this plane
crash, 67% were found to be infected with Mycoplasma, and suffered CFS-like
symptoms."
Research findings presented by Professor Kenny de Meirleir (Belgium)
to The Sydney ME / CFS Clinical and Scientific Conference, December
2001
- Sorensen B, et al. Complement activation in a model of chronic fatigue syndrome.Allergy Clin Immunol 2003 Aug;112(2):397-403
- Dr.
Levine et. al. Journal of CFS Vol. 9, #3/4, 2001
(k) Neuro-Immune Model
Morris et al. model - Infection(s), chronically activated Immune system and Neuroinflammation & Oxidative and Nitrosative stress and damage in Neurological illnesses
Activated immune pathways and inflammatory cytokines and inflammatory markers, and neuroinflammation, and high oxidative and nitrosative stress levels and damage, and mitochondria damage, damage to the nervous system, with or without infection(s) has been found in neurodegenerative diseases such as Parkinsons, Alzheimers, MS and many others. This causes extreme fatigue and tiredness. This is also found in autoimmune diseases. And they are also found in ME and CFS, a neurological illness according to WHO, with immune system dysfunctions.
- Central pathways causing fatigue in neuro-inflammatory and autoimmune illnesses. Morris et al. 2015.
- The Neuro-Immune Pathophysiology of Central and Peripheral Fatigue in Systemic Immune-Inflammatory and Neuro-Immune Diseases Morris et al. 2015.
- A neuro-immune model of Myalgic Encephalomyelitis/Chronic fatigue syndrome. Morris G, Maes M. Metab Brain Dis. 2013;28:523–40
- The Putative Role of Viruses, Bacteria, and Chronic Fungal Biotoxin Exposure in the Genesis of Intractable Fatigue Accompanied by Cognitive and Physical Disability, 2015 points to the effects of past infections and continuing chronic infections in the perpetuation of ME over many years or decades. Parvoviruses, HHV6, variants of Epstein-Barr, Cytomegalovirus, Mycoplasma, and Borrelia burgdorferi and Mold infection are mentioned. This would create some differences and subsets between patients.
- A neuro-immune model of Myalgic Encephalomyelitis/Chronic fatigue syndrome. Morris G, Maes M (2012). Metab Brain Dis. 2013 Dec;28(4):523-40.
- Morris G, Maes M. Oxidative and nitrosative stress and immune-inflammatory pathways in patients with Myalgic Encephalomyelitis (ME)/Chronic Fatigue Syndrome (CFS). Curr Neuropharmacol. 2014;12:168–85.
- Chronic fatigue syndrome: Harvey and Wessely's (bio)psychosocial model versus a bio(psychosocial) model based on inflammatory and oxidative and nitrosative stress pathways Michael Maes and Frank NM Twisk. BMC Medicine 2010, 8:35
- Morris G, Anderson G, Galecki P, Berk M, Maes M. A narrative review on the similarities and dissimilarities between myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and sickness behavior. BMC Med. 2013;11:64.
- Morris G, Maes M. Mitochondrial dysfunctions in myalgic encephalomyelitis/chronic fatigue syndrome explained by activated immuno-inflammatory, oxidative and nitrosative stress pathways. Metab Brain Dis 2014;29(1):19–36
- Myalgic encephalomyelitis/chronic fatigue syndrome and encephalomyelitis disseminata/multiple sclerosis show remarkable levels of similarity in phenomenology and neuroimmune characteristics. Gerwyn Morris and Michael Maes. Morris and Maes BMC Medicine 2013 11:205 doi:10.1186/1741-7015-11-205
- Click here to view similar research findings in MS, Alzheimers disease , Parkinsons disease, SLE, RA, Sjogrens syndrome, etc.
(m) ME outbreaks suggesting immune system abnormalities and role of viruses and other pathogens
Viruses have been isolated from the muscles of ME patients during epidemics. Using PCR methods, 50% or more of patients had evidence of such infection.
- Hyde BM.
Myalgic encephalomyelitis (chronic fatigue syndrome): an historic
perspective.
Can Dis Wkly Rep. 1991 Jan;17 Suppl 1E:5-8. PMID: 1669354
- Brodrick J.
Myalgic encephalomyelitis: yuppie 'flu--a real illness. Interview by Charlotte
Alderman.
Nurs Stand. 1990 Aug 29-Sep 4;4(49):18. PMID: 2119747
- Wilson CW.
Myalgic encephalomyelitis: an alternative theory.
J R Soc Med. 1990 Aug;
83(8):481-3. PMID: 2231572
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1292769/pdf/jrsocmed00133-0005b.pdf
- Dowsett EG, Ramsay AM, McCartney RA, Bell EJ.
Myalgic encephalomyelitis--a
persistent enteroviral infection?
Postgrad Med J. 1990 Jul;66(777):526-30.
PMID: 2170962
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2429637/pdf/postmedj00163-0031.pdf
- Lynch S, Seth R.
Depression and myalgic encephalomyelitis.
J R Soc Med. 1990 May;
83(5):341. PMID: 2380955
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1292666/pdf/jrsocmed00136-0073a.pdf
- Shepherd C.
How I treat myalgic encephalomyelitis: forum.
Practitioner. 1990 Apr 8;234
(1486):326. PMID: 2371218
- Powell S.
Myalgic encephalomyelitis.
Br J Gen Pract. 1990 Apr;40(333):170. No
abstract available. PMID: 2115368
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1371257/pdf/brjgenprac00081-0042a.pdf
- Hodson AD.
Myalgic encephalomyelitis.
J R Soc Med. 1990 Mar;83(3):199-200. PMID:
20894766
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1292588/pdf/jrsocmed00138-0079c.pdf
- Altered Distribution of Lymphocyte Populations in Chronic Fatigue Syndrome Patients. Isabel Barao, Ph.D., Daniel Peterson, M.D., Dorothy Hudig, Ph.D. Mountain West Clinical Translational Research. 2014.
- Myalgic encephalomyelitis.
J R Soc Med. 1990 Mar;83(3):199-200. No abstract
available. PMID: 2325071
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1292587/pdf/jrsocmed00138-0079b.pdf
- Prasher D, Smith A, Findley L.
Sensory and cognitive event-related potentials in myalgic
encephalomyelitis.
J Neurol Neurosurg Psychiatry. 1990 Mar;53(3):247-53. PMID:
2324756
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1014138/pdf/jnnpsyc00513-0063.pdf
- Grist NR.
Myalgic encephalomyelitis: postviral fatigue and the heart.
BMJ. 1989 Nov
11;299(6709):1219. PMID: 2513065
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1838100/pdf/bmj00258-0049b.pdf
- Lev M.
Myalgic encephalomyelitis.
J R Soc Med. 1989 Nov;82(11):693-4. PMID:
2593126
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1292388/pdf/jrsocmed00144-0069.pdf
- Sheldon, A., Habel, K., Verder, E. and
Welsh, W. Epidemic neuromyasthenia. An
outbreak of poliomyelitis-like illness in student
nurses. New England J. Med., 257: 345, 1957.
- Poskanzer, D.C., Henderson, D.A., Kunkle,
E.C., Kalter, S.S., Clement W.B. and Bland
J.O. Epidemic neuromyasthenia. An outbreak
in Punta Gorda, Florida. New England J. Med.,
257: 356, 1957.
- Deisher J.B. Benign myalgic
encephalomyelitis (Iceland disease) in Alaska.
Northwest Med., 56: 1451, 1957
- Snow P.
Myalgic encephalomyelitis.
N Z Med J. 1989 Aug 23;102(874):449.
- Murdoch JC.
The myalgic encephalomyelitis syndrome.
N Z Med J. 1989 Jul 26;102
(872):372-3. PMID: 2797553
- Coakley JH.
Myalgic encephalomyelitis and muscle fatigue.
BMJ. 1989 Jun 24;298
(6689):1711-2. PMID: 2503189
- Zala J.
Diagnosing myalgic encephalomyelitis.
Practitioner. 1989 Jun 22;233(1471):
916-9. PMID: 2594656
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1836756/pdf/bmj00237-0063d.pdf
- Myalgic encephalomyelitis.
BMJ. 1989 Jun 10;298(6687):1577-8. PMID: 2503125
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1836797/pdf/bmj00235-0051b.pdf
- Welch JC.
Abnormal erythrocytes in myalgic encephalomyelitis.
N Z Med J. 1989 Apr
26;102(866):202. PMID: 2710458
- Simpson LO.
Nondiscocytic erythrocytes in myalgic encephalomyelitis.
N Z Med J. 1989
Mar 22;102(864):126-7. PMID: 2927808
- Cant BR.
Myalgic encephalomyelitis.
N Z Med J. 1989 Feb 8;102(861):52. PMID:
2739970
- Willoughby E.
Myalgic encephalomyelitis.
N Z Med J. 1989 Jan 25;102(860):19-20.
PMID: 2913521
- Shepherd C.
Myalgic encephalomyelitis--is it a real disease?
Practitioner. 1989 Jan;233
(1461):41-2, 44, 46. PMID: 2798285
- Murdoch JC.
The myalgic encephalomyelitis syndrome.
Fam Pract. 1988 Dec;5(4):
302-6. Review. PMID: 2852613
- Myalgic encephalomyelitis.
N Z Med J. 1988 Nov 23;101(858):800-1. PMID:
3194079
- Hyde B, Bergmann S.
Akureyri disease (myalgic encephalomyelitis), forty years later.
Lancet. 1988 Nov 19;2(8621):1191-2. PMID: 2903396
- Willoughby EW.
Myalgic encephalomyelitis.
N Z Med J. 1988 Nov 9;101(857):773.
PMID: 3186037
- Spracklen FH.
The chronic fatigue syndrome (myalgic encephalomyelitis)--myth or
mystery?
S Afr Med J. 1988 Nov 5;74(9):448-52. Review. PMID: 3055363
- Myalgic encephalomyelitis.
N Z Med J. 1988 Oct 26;101(856 Pt 1):672. No abstract
available. PMID: 3186016
- Gordon N.
Myalgic encephalomyelitis.
Dev Med Child Neurol. 1988 Oct;30(5):677-82.
Review. PMID: 3068084
- Murdoch JC.
Cell-mediated immunity in patients with myalgic encephalomyelitis
syndrome.
N Z Med J. 1988 Aug 10;101(851):511-2. PMID: 3261407
- Myalgic encephalomyelitis, or what?
Lancet. 1988 Jul 9;2(8602):100-1. PMID:
2898668
- Holborow PL.
Pathophysiology of myalgic encephalomyelitis.
Med J Aust. 1988 Jun
6;148(11):598, 600. PMID: 3374430
- Lloyd AR, Wakefield D, Boughton C, Dwyer J.
What is myalgic encephalomyelitis?
Lancet. 1988 Jun 4;1(8597):1286-7. PMID: 2897549
- Archard LC, Bowles NE, Behan PO, Bell EJ, Doyle D.
Postviral fatigue syndrome:
persistence of enterovirus RNA in muscle and elevated creatine kinase.
J R Soc Med.
1988 Jun;81(6):326-9. PMID: 3404526
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1291623/pdf/jrsocmed00161-0020.pdf
- Bell EJ, McCartney RA, Riding MH.
Coxsackie B viruses and myalgic
encephalomyelitis.
J R Soc Med. 1988 Jun;81(6):329-31. PMID: 2841461
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1291624/pdf/jrsocmed00161-0023.pdf
- Jennekens FG, van Gijn J.
[Postviral fatigue syndrome or myalgic encephalomyelitis].
Ned Tijdschr Geneeskd. 1988 May 28;132(22):999-1001. Dutch. PMID: 3380192
- Wakefield D, Lloyd A, Dwyer J, Salahuddin SZ, Ablashi DV.
Human herpesvirus 6 and
myalgic encephalomyelitis.
Lancet. 1988 May 7;1(8593):1059. PMID: 2896906
- Maros K.
Myalgic encephalomyelitis?
Med J Aust. 1988 Apr 18;148(8):424. PMID:
3357477
- Lloyd A, Hanna DA, Wakefield D.
Interferon and myalgic encephalomyelitis.
Lancet. 1988 Feb 27;1(8583):471. PMID: 2893889
- Byrne E.
Idiopathic chronic fatigue and myalgia syndrome (myalgic encephalomyelitis):
some thoughts on nomenclature and aetiology.
Med J Aust. 1988 Jan 18;148(2):80-2.
PMID: 3336341
- Ho-Yen DO, Carrington D, Armstrong AA.
Myalgic encephalomyelitis and alpha-
interferon.
Lancet. 1988 Jan 16;1(8577):125. PMID: 2891971
- Behan PO, Behan WM.
Postviral fatigue syndrome.
Crit Rev Neurobiol. 1988;4(2):
157-78. Review. PMID: 3063394
- Matthew C.
Myalgic encephalomyelitis and the doctor.
N Z Med J. 1987 Sep 9;100(831):
569. PMID: 3451147
- Mukherjee TM, Smith K, Maros K.
Abnormal red-blood-cell morphology in myalgic
encephalomyelitis.
Lancet. 1987 Aug 8;2(8554):328-9. PMID: 2886780
- Archer MI.
The post-viral syndrome: a review.
J R Coll Gen Pract. 1987 May;37(298):
212-4. Review. PMID: 3320358
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1710789/pdf/jroyalcgprac00029-0021.pdf
- Matthew C.
Myalgic encephalomyelitis.
N Z Med J. 1986 Sep 10;99(809):678. PMID:
3463904
- Blackmore RJ.
Myalgic encephalomyelitis and Immunovir.
N Z Med J. 1986 Jul 9;99
(805):513. PMID: 3461389
- McCartney RA, Banatvala JE, Bell EJ.
Routine use of mu-antibody-capture ELISA for
the serological diagnosis of Coxsackie B virus infections.
J Med Virol. 1986 Jul;19(3):
205-12. PMID: 3016163
- Simpson LO, Shand BI, Olds RJ.
Blood rheology and myalgic encephalomyelitis: a pilot
study.
Pathology. 1986 Apr;18(2):190-2. PMID: 3093959
- Rowlandson PH, Stephens JA.
Cutaneous reflex responses recorded in children with
various neurological disorders.
Dev Med Child Neurol. 1985 Aug;27(4):434-47.
PMID: 2993087
- Staines D.
Myalgic encephalomyelitis hypothesis.
Med J Aust. 1985 Jul 22;143(2):91.
PMID: 4021881
- Byrne E, Trounce I, Dennett X.
Chronic relapsing myalgia (Post viral): clinical,
histological, and biochemical studies.
Aust N Z J Med. 1985 Jun;15(3):305-8. PMID:
3864422
- Maurizi CP.
Raphe nucleus encephalopathy (myalgic encephalomyelitis, epidemic
neuromyasthenia).
Med Hypotheses. 1985 Apr;16(4):351-4. PMID: 4010573
- Myalgic encephalomyelitis.
N Z Med J. 1985 Jan 23;98(771):20-1. PMID: 3855509
- Gow PJ.
Myalgic encephalomyelitis.
N Z Med J. 1984 Dec 12;97(769):868. PMID:
6595571
- Myalgic encephalomyelitis.
N Z Med J. 1984 Nov 14;97(767):782. PMID: 6593632
- Myalgic encephalomyelitis.
N Z Med J. 1984 Oct 10;97(765):698-9. PMID:
6592485
- Bell EJ, McCartney RA.
A study of Coxsackie B virus infections, 1972-1983.
J Hyg
(Lond). 1984 Oct;93(2):197-203. PMID: 6094660
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2129449/pdf/jhyg00014-0036.pdf
- Gow PJ.
Myalgic encephalomyelitis.
N Z Med J. 1984 Sep 12;97(763):620. PMID:
6591048
- Calder BD, Warnock PJ.
Coxsackie B infection in a Scottish general practice.
J R Coll
Gen Pract. 1984 Jan;34(258):15-9. PMID: 6319691
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1959663/pdf/jroyalcgprac00169-0017.pdf
- Keighley BD, Bell EJ.
Sporadic myalgic encephalomyelitis in a rural practice.
J R Coll
Gen Pract. 1983 Jun;33(251):339-41. PMID: 6310105
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1972871/pdf/jroyalcgprac00078-0021.pdf
- Fegan KG, Behan PO, Bell EJ.
Myalgic encephalomyelitis--report of an epidemic.
J R
Coll Gen Pract. 1983 Jun;33(251):335-7. PMID: 6310104
- Know your organizations: the Myalgic Encephalomyelitis Association.
Health Visit.
1982 Jul;55(7):350. PMID: 6921182
- Parish G.
Myalgic encephalomyelitis: faulty fibres?
Nurs Mirror. 1981 Oct 7;153(15):
41-2. PMID: 6913031
- Ramsay M.
Myalgic encephalomyelitis: a baffling syndrome.
Nurs Mirror. 1981 Oct
7;153(15):40-1. PMID: 6913030
- Parish JG.
Myalgic encephalomyelitis.
Lancet. 1981 Apr 25;1(8226):950-1. PMID:
6112360
- Layzer RB.
Myoglobinaemia in benign myalgic encephalomyelitis.
Lancet. 1981 Mar
21;1(8221):670. PMID: 6110899
- Goodwin CS.
Was it benign myalgic encephalomyelitis?
Lancet. 1981 Jan 3;1(8210):
37-8. PMID: 6109065
- May PG, Donnan SP, Ashton JR, Ogilvie MM, Rolles CJ.
Personality and medical
perception in benign myalgic encephalomyelitis.
Lancet. 1980 Nov 22;2(8204):1122-4.
PMID: 6107734
- Church AJ.
Myalgic encephalomyelitis.
Med J Aust. 1980 Aug 23;2(4):224. PMID:
7432298
- Behan PO.
Epidemic myalgic encephalomyelitis.
Practitioner. 1980 Aug;224(1346):
805-7. PMID: 7433399
- Bishop J.
Epidemic myalgic encephalomyelitis.
Med J Aust. 1980 Jun 14;1(12):585-6,
609. PMID: 7402153
- Ramsay AM, Rundle A.
Clinical and biochemical findings in ten patients with benign
myalgic encephalomyelitis.
Postgrad Med J. 1979 Dec;55(654):856-7. PMID: 548947 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2425703/?tool=pubmed
- Pampiglione G, Harris R, Kennedy J.
Electro-encephalographic investigations in
myalgic encephalomyelitis.
Postgrad Med J. 1978 Nov;54(637):752-4. PMID: 746023
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1606252/pdf/brmedj00135-0058a.pdf
- Behan PO.
Post-infectious encephalomyelitis: some aetiological mechanisms.
Postgrad
Med J. 1978 Nov;54(637):755-9. PMID: 34143
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1606252/pdf/brmedj00135-0058a.pdf
- Wookey C.
Epidemic myalgic encephalomyelitis.
Br Med J. 1978 Jul 15;2(6131):202.
PMID: 678851
- Epidemic myalgic encephalomyelitis.
Br Med J. 1978 Jun 3;1(6125):1436-7.
PMID: 647324
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1604957/pdf/brmedj00128-0006b.pdf
- Ramsay AM, Dowsett EG, Dadswell JV, Lyle WH, Parish JG.
Icelandic disease (benign
myalgic encephalomyelitis or Royal Free disease)
Br Med J. 1977 May 21;1(6072):
1350. PMID: 861618
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1607215/pdf/brmedj00463-0058b.pdf
- Parish JG.
Benign myalgic encephalomyelitis.
Br J Psychiatry. 1973 Jun;122(571):735.
PMID: 4716076
- Ramsay AM.
Benign myalgic encephalomyelitis.
Br J Psychiatry. 1973 May;122(570):
618-9. PMID: 4717041
- Walther H.
[Epidemic myalgic encephalomyelitis].
Schweiz Rundsch Med Prax. 1972
Apr 11;61(15):469-80. German. PMID: 5022278
- Benign myalgic encephalomyelitis.
Med J Aust. 1970 Jul 4;2(1):3. PMID: 5447847
- Lyle WH.
Encephalomyelitis resembling benign myalgic encephalomyelitis.
Lancet.
1970 May 23;1(7656):1118-9. PMID: 4191997
- Innes SG.
Encephalomyelitis resembling benign myalgic encephalomyelitis.
Lancet.
1970 May 9;1(7654):969-71. PMID: 4191935
- Mourad S, Chidiac J.
Benign myalgic encephalomyelitis in Lebanon.
J Med Liban.
1969;22(6):735-40. PMID: 5370523
- Kendell RE.
The psychiatric sequelae of benign myalgic encephalomyelitis.
Br J
Psychiatry. 1967 Aug;113(501):833-40. PMID: 6048369
- Gsell O.
[Benign myalgic encephalomyelitis, epidemic pseudoneurasthenia].
Schweiz
Med Wochenschr. 1963 Feb 2;93:197-200. German. PMID: 13950994
- Price JL.
Myalgic encephalomyelitis.
Lancet. 1961 Apr 8;1(7180):737-8. PMID:
13737972
- Pool JH, Walton JN, Brewis EG, Uldall PR, Wright AE, Gardner PS.
Benign myalgic
encephalomyelitis in Newcastle upon Tyne.
Lancet. 1961 Apr 8;1(7180):733-7. PMID:
13737057
- Klajman A, Pinkhas B, Rannon L.
[An outbreak of an epidemic of benign myalgic
encephalomyelitis].
Harefuah. 1960 May 15;58:314-5. Hebrew. PMID: 14409571
- Bornstein B, Bechar M, Lass H.
Benign myalgic encephalomyelitis. (Report of five
cases).
Psychiatr Neurol (Basel). 1960 Mar;139:132-40. PMID: 13802904
- Daikos GK, Garzonis S, Paleologue A, Bousvaros GA, Papadoyannakis N.
Benign
myalgic encephalomyelitis: an outbreak in a nurses' school in Athens.
Lancet. 1959 Apr
4;1(7075):693-6. PMID: 13642848
- Acheson ED.
The clinical syndrome variously called benign myalgic encephalomyelitis,
Iceland disease and epidemic neuromyasthenia.
Am J Med. 1959 Apr;26(4):569-95.
PMID: 13637100
http://www.meresearch.org.uk/information/keypubs/Acheson_AmJMed.pdf
- Bhatia BB, Chandra S, Bhushan C.
Benign myalgic encephalomyelitis.
J Indiana State
Med Assoc. 1958 Oct;31(8):327-8. PMID: 13611265
- Gsell O.
[Encephalitis myalgica epidemica, a poliomyelitis-like disease; epidemic
neuromyasthenia, benign myalgic encephalomyelitis].
Schweiz Med Wochenschr. 1958
May 17;88(20):488-91. German. PMID: 13568694
- Greene IM.
Benign myalgic encephalomyelitis; syndrome mimicking anterior
poliomyelitis.
J Fla Med Assoc. 1958 Apr;44(10):1105-6. PMID: 13525606
- Galpin JF.
Benign myalgic encephalomyelitis.
Br J Clin Pract. 1958 Mar;12(3):186-8
passim. PMID: 13510534
- Deisher JB.
Benign myalgic encephalomyelitis (Iceland disease) in Alaska.
Northwest
Med. 1957 Dec;56(12):1451-6. PMID: 13484090
- [Benign epidemic myalgic encephalomyelitis].
Recenti Prog Med. 1957 Nov;23(5):
525-31. Italian. PMID: 13518620
- EPIDEMIC myalgic encephalomyelitis.
Br Med J. 1957 Oct 19;2(5050):927-8.
PMID: 13472011
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1962482/pdf/brmedj03125-0047.pdf
- Acheson ED.
Benign myalgic encephalomyelitis.
Lancet. 1957 Apr 20;272(6973):834-5.
PMID: 13417614
- Galpine JF, Brady C.
Benign myalgic encephalomyelitis.
Lancet. 1957 Apr 13;272
(6972):757-8. PMID: 13417586
- Lindan R.
Benign Myalgic Encephalomyelitis.
Can Med Assoc J. 1956 Oct 1;75(7):
596-7. PMID: 20325349
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1824640/pdf/canmedaj00742-0051.pdf
- Blattner RJ.
Benign myalgic encephalomyelitis (Akureyri disease, Iceland disease).
J
Pediatr. 1956 Oct;49(4):504-6. PMID: 13358047
- A new Clinical Entity ? Lancet 1956
- Outbreak at the Royal Free.
E.D Acheson. The Lancet, Volume 266, Issue 6886, Pages 394 - 395, 20 August 1955.
Years of Epidemics
1917 Van Economo reports an illness involving brain and neurological inflammation and great fatigue and some deaths. See paper 'New Clinical Entity' published in the Lancet in 1956.
1918 - 1924, several outbreaks of an illness involving brain and neurological inflammation and fatigue reported throughout Europe. See paper 'New Clinical Entity' published in the Lancet in 1956.
1924 England and Wales 5,039 cases of encephalitis lethargica. See paper 'New Clinical Entity' published in the Lancet in 1956.
1934
Los Angeles County Hospital. Called 'Atypical Poliomyelitis'
1936
Fond Du Lac, Wisconsin - St. Agnes Convent - Encephalitis
1937
Erstfeld, Switzerland -
Abortive Poliomyelitis
1937
St. Gallen, Switzerland
- Frohburg Hospital – Abortive Poliomyelitis
1939
Middlesex, England - Harefield Sanatorium
1939
Degersheim, Switzerland - Abortive Poliomyelitis
1945
Pennsylvania. Hospital of the University of Pennsylvania - epidemic Pleurodynia
1946
Iceland
disease resembling Poliomyelitis with the character of Akureyri disease
1948
Iceland, North Coast towns - epidemic simulating Poliomyelitis
1949
Adelaide, South Australia - a disease resembling Poliomyelitis
1949 Cambridgeshire, England -
aberrant poliomyelitis. Involvement of other Enteroviruses suspected.
1950
Louisville, Kentucky -- St. Joseph
's Infirmary - epidemic Neuromyasthenia
1950
Upper State New York -- outbreak resembling the
Iceland disease, simulating
"
acute Anterior Poliomyelitis
1952
London, England - Middlesex Hospital Nurses
'
Home - Encephalomyelitis
associated with Poliomyelitis virus
1952
Copenhagen, Denmark - epidemic Myositis
1952
Lakeland, Florida - epidemic Neuromyasthenia
1953
Coventry and District, England - an illness resembling Poliomyelitis observed in
nurses
1953
Rockville, Maryland - Chestnut Lodge Hospital - Poliomyelitis-like epidemic
Neuromyasthenia
1953
Jutland, Denmark - epidemic Encephalitis with vertigo
1954 Seward, Alaska - benign Myalgic Encephalomyelitis (Iceland Disease)
1954
Berlin, Germany - British army - further outbreak of a disease resembling
Poliomyelitis
1954
Liverpool, England - outbreak among medical and nursing staff in a local
hospital
1955
Dalston, Cumbria, England – epidemic and sporadic outbreak of an unusual
disease
1955
London, England - Royal Free Hospital - outbreak in staff and patients of Benign
Myalgic Encephalomyelitis
1955 Hampstead, London
1955
Perth, Australia - virus epidemic in waves
1955
Gilfac Goch, Wales - outbreak of benign Myalgic Encephalomyelitis
1955
Durban City, South Africa - Addington Hospital - outbreak among nurses of Durban Mystery Disease
1955
Segbwema, Sierra Leone - outbreak of Encephalomyelitis
1955
Patreksfjorour and Porshofn, Iceland - unusual response to polio vaccine
1955
Northwest London, England - nurses
'
residential home - acute Infective
Encephalomyelitis simulating poliomyelitis
1956
Ridgefield, Connecticut - epidemic Neuromyasthenia
1956
Punta Gorda Florida - outbreak of epidemic Neuromyasthenia
1956
Newton-le-Willows, Lancashire, England - Lymphocytic Meningoencephalitis with
myalgia and rash
1956
Pittsfield and Williamstown, Massachusetts - benign Myalgic Encephalomyelitis
1956
Coventry, England - epidemic malaise, benign Myalgic Encephalomyelitis
1957
Brighton, South Australia - Cocksakie Echo virus Meningitis, epidemic Myalgic
Encephalomyelitis
1958
Athens, Greece - nurses
'
school - outbreak of benign Myalgic Encephalomyelitis
with periostitis and arthopathy noted.
1958
Southwest London, England - reports of sporadic cases of Myalgic
Encephalomyelitis
1959
Newcastle Upon Tyne, England - outbreak of benign Myalgic Encephalomyelitis
1961
Basel, Switzerland - sporadic cases of benign Myalgic Encephalomyelitis
1961
New York State - outbreak of epidemic Neuromyasthenia in a convent
1964
Northwest London, England - epidemic malaise, epidemic Neuromyasthenia
1964
Franklin, Kentucky - outbreak of Neuromyasthenia in a factory
1967
Edinburgh, Scotland - sporadic cases resembling benign Myalgic
Encephalomyelitis
1968
"
Fraidek, Lebanon - benign Myalgic Encephalomyelitis
1969
Brooklyn, New York - State University of New York Downstate Medical Center -
epidemic Neuromyasthenia, unidentified symptom complex
1970
Lackland Air Force Base, Texas - epidemic Neuromyasthenia
1970
London, England - Great Ormond Street Hospital for Children - outbreak of
Neuromyasthenia among nurses
1975
Sacramento, California - Mercy San Juan Hospital - Infectious Venulitis, epidemic
"
Phelobodynia
1976
Southwest Ireland - epidemic Neuromyasthenia, benign Myalgic
Encephalomyelitis
1977
Dallas – Fort Worth, Texas - epidemic Neuromyasthenia
1979
Southampton, England - Myalgic Encephalomyelitis
1980
West Kilbridge, Ayrshire, Scotland - epidemic Myalgic Encephalomyelitis
1980
San Francisco, California – epidemic persistent flu-like illness
1981
Stirlingshire, Scotland
- sporadic Myalgic Encephalomyelitis
1982
West Otago, Dunedin and Hamilton, New Zealand - Myalgic Encephalomyelitis
1983
Los Angeles, California - initial cases of an unknown, chronic symptom complex
involving profound "fatigue"
1984
Lake Tahoe Area of California/Nevada - start of a yearlong epidemic involving
"
over 160 cases of chronic illness eventually characterized as Chronic Fatigue
Syndrome
Source: Paradigm Change web site
|

