| Heart function and activity : Cardiomyopathy, PFO abnormality, Diastolic Dysfunction and Increased risk of Heart attack in ME patients
Scientific and Medical Evidence
Cardiac
and Vascular and Blood vessel problems. Increased risk of heart attack
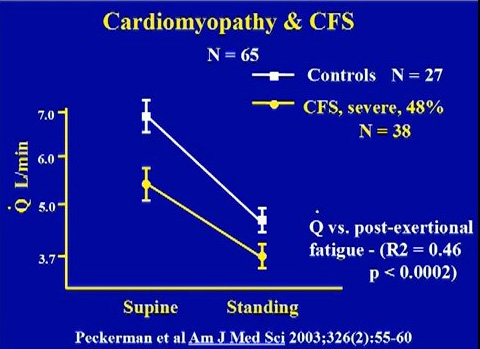
Peckerman A, et al. Abnormal impedance cardiography predicts symptom severity in chronic fatigue syndrome. Am J Med Sci 2003 Aug;326(2):55-60.
Dr. Martin Lerner's lecture on clinical findings
Video lecture by Dr. Paul Cheney on cardiomyopathy findings in ME
Markedly Impaired Cardiac Function in Chronic Fatigue Syndrome. Hollingsworth KG, Hodgson T, Macgowan GA, Blamire AM, Newton JL.: J Intern Med. 2011 Jul 27.
Research shows that ME patients have serious heart and vascular abnormalities arising from ME, making them highly susceptible to a sudden heart attack. Many ME patients have died prematurely of heart attacks - Patient deaths from ME
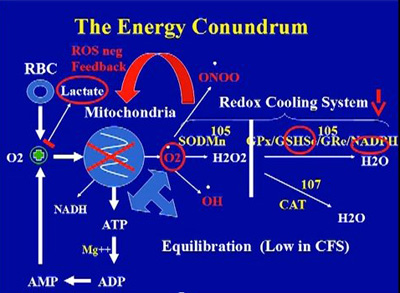
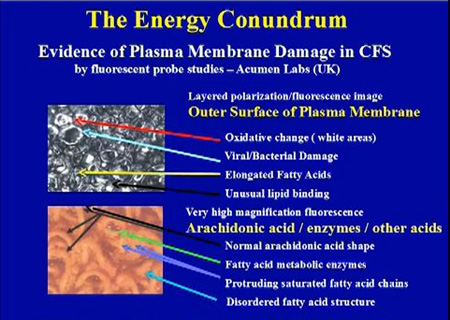
Cardiomyopathy arising from mitochondria dysfunction, oxidative stress and infections
Reduced cardiac fillng, long IVRT, low cardiac output as a
result of mitochondria dysfunctions, infections (some cases),
toxins build up,
and damage caused by high oxidative and nitrosative
stress levels
over time. A very consistent finding in his medical practice.
Dr. Paul Cheney , The Cheney Clinic, US
Source: Dr. Paul Cheney, The Cheney Clinic, USA.
Source: Dr. Paul Cheney, The Cheney Clinic, USA
- Dr. Paul Cheney
- Important Cardiac and Mitochondria findings in ME and CFS
- Video lecture by Dr. Paul Cheney on cardiomyopathy findings in ME
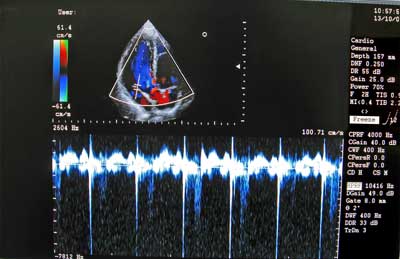
- Dr. Paul Cheney uses 3D echocardiograph machine, Impedance cardiography and Doppler Ultrasound technology in his medical clinic.
Test for low Q and test for normal circulation and micro-cirulation to the body's ogans. “Q” stands for cardiac output in litres per minute. This is most consistent finding in ME. Under conditions of low Q the body sacrifices tissue perfusion in order to maintain blood pressure according to Dr. Paul Cheney and Dr. Peckerman. The combination of low Q and reduced circulation has multiple adverse effects on other organs and the body.
Diastolic dysfuncton, abnormally long IVRT, low cardiac output with a cardiac index (CI) of less than 3.0, where normal is 3.0 - 3.5. Dr. Cheney states “I have yet to see a 3-D CI above 2.8, and the average is 1.8 in my practice which sits at the cardiogenic shock threshold".
- Redox Control
"All CFS cases are toxic to oxygen by echo derived IVRT response criteria as against 1/3 of healthy controls who are mildly toxic to oxygen but when probed carefully are not as healthy as they purport to be."
Dr. Paul Cheney, The Cheney Clinic, USA.
- Test for oxygen toxicity by echo derived IVRT response criteria.
- Test for poor or defective redox control. Poor redox control is found in most ME patients and is related to mitochondrial dysfunctions. It may also be responsble for low sedimentation rates due to oxidative damage to blood cells. These tests are highly recommended by Dr. Paul Cheney.
- Test for
low GSH/GSSG ratios, low NADPH, low SOD or GPx function. Dr. Cheney typically finds
low GSH/GSSG ratios, low NADPH, low SOD or GPx function in his medical practice.
- Reduced sedimentation rate suggesting induced Haemoglobinopathy. (Dr. Paul Cheney)
- Due to the heightened risk of a heart attack in ME patients, all patients who have had ME for 1 year or more should have a Impedance cardiography to assess cardiac function, rhythm and activity. This can be carried out in a major hospital, under the supervision of a Cardiologist. This may require a few visits to the hospital. Test results will determine further action / treatments.
- Test for low blood volume and Central diabetes insipidus
- Test for Intracellular Magnesium and Potassium Deficiencies
- Heart and Cardiac dysfunctions arising from chronic inflammatory immune response to Molds and Mycotoxins:
Vasoactive intestinal polypeptide (VIP) treatment for person
ELISA test of urine. Brewer JH, Thrasher JD, Straus DC, Madison RA, Hooper D. Detection of Mycotoxins in Patients with Chronic Fatigue Syndrome. Toxins. 2013; 5(4):605-617
- Dr. Dan Peterson
- A characteristic repetitively oscillating T-wave inversions
and/or T-wave flattening during 24 hour monitoring
- Decreased vagal activity
- Orthostatic Intolerance
–
POTS
–
Neurally mediated hypotension
- Decreased total blood volume
- Lower blood pressure and abnormal diurnal blood
pressure regulation
- Reduced cardiac stroke volume and cardiac output
- Dr. Byron Hyde one of the top ME doctors in the world recommends several cardiac tests for ME
- Cardiac Diagnostic Tests
- Dr. Byron Hyde also recommends the following tests on all patients
- Visual carotid Doppler from aortic arch
- Visual transcranial Doppler to include vertebral and basilar arteries
- Thyroid ultrasound
- Echocardiogram and Doppler
- 24-hour Holter monitor
- Stress ECG or chemical stress test
- Cardiac PET scan
- Circulating red blood cell and serum volume
Excerpt from The Complexities of Diagnosis By Dr. Byron Hyde, Chairman, Nightingale Research Foundation, Chapter 3 in
Handbook of Chronic Fatigue Syndrome. Leonard A. Jason, Patricia A. Fennell, Renée R. Taylor
' Dr. John Richardson from Newcastle upon Tyne has followed ME patients in Durham and
Northumberland counties of the United Kingdom for three to four generations. I am aware of no other
physician in the world with such a historic view of ME patients. He has repeatedly demonstrated that
many ME patients go on to develop structural heart injury. The injury is usually valvular or related to
pericardial effusion, and although most settle down, some do not and may develop myopathy. So I started
to look at the hearts of these patients.
I have found that during the first year of acute onset ME/CFS disability, the incidence of
pericardial effusion is unusually high. This seems to settle down with no apparent short-term problem,
and after a year, the cases of pericardial fluid decrease considerably. However, the incidence of valvular
disease in people in their 30s and 40s appears to be higher than in the normal population. When I find a
significant valvular injury, I then repeat the echocardiogram yearly, and more frequently if the patient
develops shortness of breath. I have observed several cases of elevated right heart pressure, significant
septal defects, and increased myocardial wall thickening. Some who have had the injured valve replaced
have miraculously returned to normal health. Are these incidental findings? I do not know, but Dr.
Richardson has identified more than several hundred cardiopathies in his ME practice. I had two heart
valve replacements in this group in the past year out of a total of 50 new patients.
Carotid and Transcranial Doppler Few physicians investigating ME/CFS employ the visual carotid and transcranial Doppler. This is a major error. It is a relatively inexpensive and totally safe procedure that does things no other type of test can do. On rare occasions, you will find aneurysms and subclavian steal anomaly with this test. Carotid atherosclerosis – sometimes substantial – is often found in
patients with lipid dysfunction. This is a treatable condition and can be part of the cause of a CNS fatigue
syndrome. You may say that any internist or cardiologist can pick up carotid pathology with a stethoscope, but few do who do not have an office Doppler. The carotid scan is also essential if you wish
to do a transcranial Doppler. I examined a patient from the United States who had been diagnosed as having CFS in two major
U.S. CFS clinics. She was given alternative medications and told to return in one year. She had complete
obstruction of the vertebral basilar arteries and approximately 80% and 90% obstruction in either carotid.
I was amazed that she was still alive. She was successfully operated on in Boston and her CFS has
significantly improved.
The transcranial Doppler is not a perfect test. Patients with small foramen magnum space are
difficult to visualize. But it will demonstrate high level internal carotid and other arterial obstruction that
is beyond the normal range of a stethoscope. Only rarely do I get the chance to investigate posttraumatic
mitral valve area (MVA) patients who develop an acute fatigue syndrome where personality or
intellectual change has given rise to the diagnosis of CFS. In two of the past four such patients, I have
demonstrated small subcortical arterial blowouts that had been missed by neurologists and that were
possibly the cause of their pathophysiology.
In patients with ME/CFS, it is possible to demonstrate spasmodic disease of both major and
smaller arteries with no typical evidence of migraine. This arterial pathology may be the end organ
underlying cause of some ME patients' illness. Often MRls and MRAs miss such arterial physiological
pathology. Why? The technology of the MRA consists of a receiving computer revolving around the brain
that may only give a picture of the maximum arterial diameter. In other words, what you see on the MRA
is not reality but one view of reality. With the transcranial Doppler, the operator actually watches and
films the kinetic movement of the arteries within the brain and can measure the velocity of the blood
flow. Not only can you see these arteries move; if they are in spasm, you can observe this as well. Like
ME/CFS muscles, ME brains are sometimes in significant pathological spasm. This knowledge may lead
to more effective treatments of ME/CFS disease. Arterial spasm may account for some, but not all, of the
SPECT changes that are routinely seen in ME patients.
I often find partial or complete vertebral or basilar artery obstruction. Frequently, I find left
middle cerebral artery spasm or obstruction and, less frequently, frontal artery spasm in ME/CFS patients
who do not report a migraine history. Left middle cerebral arterial field hypoperfusion is typical of ME. '
- Dr. Martin Lerner, a well known ME specialist in the USA has found the following heart abnormalities in patients with ME
- Abnormal Holter Monitoring Oscillating T-wave Flattening and Inversions
- Tachycardia at Rest
- Left Ventricular (LV) Dilatation
- Decreased LV Ejection Fraction
- Pathologic / Cardiomyopathy / Apoptosis (Lytic Replication Produces Myocarditis with Cellular Inflammatory Response)
- 24-hour Holter ECG. The T-wave (the waves are called P, Q, R, S, and the last one is T) is normally a peak, and then the wave levels off and starts with the P-wave again. In chronic fatigue and fibromyalgia patients, the T-wave flattens off, or actually inverts. That means the blood in the left ventricle is not being squeezed up through the aorta and around through the body.
-
Heart Arrrhythmias
- Test for Vasculitis. (Dr. Byron Hyde)
- Cardiac morphology and function assessment using magnetic resonance imaging and cardiac tagging methodology
- Dr. Julia Newton is using new heart monitoring techniques for ME. She has found the following - “CFS patients have markedly reduced cardiac mass and blood pool volumes, particularly end diastolic volume: this results in significant impairments in stroke volume and cardiac output compared to controls.” Source: Hollingsworth, K. G., Hodgson, T., MacGowan, G. A., Blamire, A. M. and Newton, J. L. (2012), Impaired cardiac function in chronic fatigue syndrome measured using magnetic resonance cardiac tagging. Journal of Internal Medicine, 271: 264–270.
|

